Copy to clipboard
Copy to clipboard 
Value-based healthcare is driving today’s business decisions, from people to place of surgery to product. The OMTEC® 2017 opening Keynote Panel affirmed that fact as they predicted the companies and technologies that will lead orthopaedics in 2025. No matter which size or market segment, success will come to companies that are able to assist hospital and surgeon customers in sketching out the myriad ways that value can be drawn.
Industry shifts discussed by the panel included size and roles of salesforces, the move of procedures to outpatient settings and the adoption of additive manufacturing. Let’s review how those changes are playing out.
First, I’d like to say that these initiatives may sound repetitive to you. Each has been discussed by industry for years and implemented to various degrees. It’s important to remember, though, that it will take your customers years to implement value-based decision making. The concept is evolutionary. As hospital and surgeon customers change, so will the demands placed upon the orthopaedic supply chain.
Our panel consisted of these thought-leaders:
Sales Reps
The role of the sales rep will continue to be redefined as cost is scrutinized throughout the entire delivery system. The consensus of the panel was that by 2025, there will be fewer sales reps and their responsibilities will have changed.
The conversation began with Smith & Nephew’s launch of Syncera in 2014. While Smith & Nephew leadership has stated that the model continues to capture business, its revenue, profitability and clinical outcomes remain unknown.
Panelists commented that they expect more companies to roll out differentiated service models with the ultimate goal of decreasing the cost associated with sales and inventory management.
In considering the primary functions of a sales rep—surgeon nurturing, surgical guiding and inventory fielding—one suggestion was for companies to take a tiered approach whereby a set of reps supports simpler cases and logistics, while remaining reps take on more complex cases and convert accounts.
Dr. Bruder equated it to a hunter/gatherer and farmer mentality. Mr. Lohrer noted that he has seen DePuy Synthes begin to execute on such a model.
To eliminate the sales reps’ downtime, Dr. Bruder predicted that companies with broad portfolios across market segments would boost the array of products that a rep supports, meaning that sales reps would not specialize in one product or anatomical region.
Mr. Rose believes that there will be fewer quota-carrying reps in orthopaedics by 2025. “Bringing this theme back to value-based healthcare, it gives the companies an opportunity to have a conversation with their hospitals, because they are basically getting a free scrub tech or a free PA based on the amount of cases these high-performing sales reps see and the knowledge they have with ten to 20+ years in the OR. If [the hospital] doesn’t want to pay for that rep, they don’t have to. If they do want that rep there, it’s going to come with a different service model. That evolution will occur.”
Panelists did not dispute the value that sales reps bring to their companies and to the surgeon. As we have learned from previous conversations, industry sales leaders and consultants believe that the great sales reps will become more valuable as companies condense their forces. Additionally, while a portion of the market could be served under a repless model, companies would need to invest in technology and resources to ensure that outcomes are maintained.
Mr. Lohrer commented that removing the rep altogether would require foolproof technology, like a kit with one implant, minimal instrumentation, a technique guide and perhaps even a set staff to assist the surgeon. Keep an eye on the niche market of disposable or single-use systems currently found in spine and trauma.
Companies will take different approaches based on size, but there is an appetite at the hospital and device company level to play with salesforce dynamics.
Outpatient Procedures
The movement of procedures to ambulatory surgery centers (ASCs) is on the rise thanks to a number of factors, including the desire of payors and providers to decrease episode costs, and surgeons to maintain their autonomy in product preference. The increase in ASC procedures for spine, knee and hip—the three largest market segments, by our estimates—is in the hundreds of percents. The ASC could be a prime opportunity for small and medium-sized companies to compete.
Procedures performed in the outpatient setting are more predictable and require a smaller range of implants and instruments, Mr. Rose said. This could decrease the amount of capital spent on launching a new system, and could allow companies to scale faster and more efficiently.
“If [your company is] starting small, you don’t have a lot of revenue, a lot of infrastructure, a lot of reps, so I think it’s an opportunity to look at a problem in a different way,” Mr. Lohrer said. “In the U.S., Lima has a tiny market share. We’re pretty open. We’re not too worried about price levels. We know there are different kinds of customers, and we can think relatively freely about going to an ASC. Ten years ago, when I was a Synthes sales rep, that was not the case. I had the ASC, and then 200 yards away I had the hospital. I was worried about them finding out about each other’s different pricing levels. It’s a much more complicated relationship. For the small guys, it’s an opportunity to do what makes sense without worrying about what you’re losing.”
Reimbursement remains a challenge in the outpatient setting. Our conversations with spine and joint reconstruction surgeons in urban areas on both coasts have indicated that payors are beginning to incentivize surgeons who are able to demonstrate improved clinical and economic outcomes for ASC procedures. But work remains. For example, Medicare does not cover total hip or total joint procedures in the outpatient setting.
Mr. Rose reminded the audience that ASCs do require a higher level of service. There is often a closer relationship with sales reps and surgeons to ensure that the proper inventory is on hand, and there is an efficiency to surgeries that allows the ASC to turn over the operating room more quickly than in a hospital.
This observation from Mr. Rose aligns with our conversations with surgeons. For example, one ASC in particular requires two sets of instruments two days in advance of the surgery.
Additive Manufacturing
Orthopaedics’ adoption of additive manufacturing has created three groups: those that are fully invested and believe it can be revolutionary to the industry, those that have invested without a clear understanding of how the technology will ultimately be used, and those that are standing on the outside waiting for proof.
The consensus of the panel was that the technology’s benefits in device design, customization and bony ingrowth are proven. However, speed and cost remain large barriers to move the technology from niche to mainstream, and even then there was hesitation to say that it could be a player as a traditional manufacturing process by 2025.
Areas in which it could be helpful include customization for revisions or deformities, and even instrument manufacturing.
Dr. Bruder mentioned that Amendia 3D-prints instruments, which is a simpler process than printing devices. A surgeon can describe the length and dimensions of his preferred screwdriver, and the manufacturer can satisfy the surgeon in a way that doesn’t involve the complexity and liability of regulations associated with implants.
Incidentally, just hours before the panel convened, Stryker and GE—two of the larger players in additive—announced a materials, machine and supply chain partnership to support Stryker’s growth.
Mr. Rose, the most bullish of the bunch, pointed to ConforMIS’ and Stryker’s successes with additive products in total knee replacement.
“Recently, I heard an investor say, ‘Most people tend to overestimate change in the near term and underestimate change in the long term,’ ” he said. “It would be naïve to think that there’s not an opportunity to put a 3D printer in a hospital in ten or 15 years, and [device companies] can move some of the manufacturing closer to point of care. At the same time, I think we’re still very early in the stages of realizing what this technology is capable of in the long term, from a commercial standpoint.”
The panel discussed additional trends like robotics and episode-of-care solutions. Mr. Lohrer left the audience with the smart comment that in identifying trends and setting priorities, “You cannot lose track of growing your business.”
Carolyn LaWell is ORTHOWORLD’s Chief Content Officer. She can be reached by email.
Value-based healthcare is driving today’s business decisions, from people to place of surgery to product. The OMTEC® 2017 opening Keynote Panel affirmed that fact as they predicted the companies and technologies that will lead orthopaedics in 2025. No matter which size or market segment, success will come to companies that are able to assist...
Value-based healthcare is driving today’s business decisions, from people to place of surgery to product. The OMTEC® 2017 opening Keynote Panel affirmed that fact as they predicted the companies and technologies that will lead orthopaedics in 2025. No matter which size or market segment, success will come to companies that are able to assist hospital and surgeon customers in sketching out the myriad ways that value can be drawn.
Industry shifts discussed by the panel included size and roles of salesforces, the move of procedures to outpatient settings and the adoption of additive manufacturing. Let’s review how those changes are playing out.
First, I’d like to say that these initiatives may sound repetitive to you. Each has been discussed by industry for years and implemented to various degrees. It’s important to remember, though, that it will take your customers years to implement value-based decision making. The concept is evolutionary. As hospital and surgeon customers change, so will the demands placed upon the orthopaedic supply chain.
Our panel consisted of these thought-leaders:
Sales Reps
The role of the sales rep will continue to be redefined as cost is scrutinized throughout the entire delivery system. The consensus of the panel was that by 2025, there will be fewer sales reps and their responsibilities will have changed.
The conversation began with Smith & Nephew’s launch of Syncera in 2014. While Smith & Nephew leadership has stated that the model continues to capture business, its revenue, profitability and clinical outcomes remain unknown.
Panelists commented that they expect more companies to roll out differentiated service models with the ultimate goal of decreasing the cost associated with sales and inventory management.
In considering the primary functions of a sales rep—surgeon nurturing, surgical guiding and inventory fielding—one suggestion was for companies to take a tiered approach whereby a set of reps supports simpler cases and logistics, while remaining reps take on more complex cases and convert accounts.
Dr. Bruder equated it to a hunter/gatherer and farmer mentality. Mr. Lohrer noted that he has seen DePuy Synthes begin to execute on such a model.
To eliminate the sales reps’ downtime, Dr. Bruder predicted that companies with broad portfolios across market segments would boost the array of products that a rep supports, meaning that sales reps would not specialize in one product or anatomical region.
Mr. Rose believes that there will be fewer quota-carrying reps in orthopaedics by 2025. “Bringing this theme back to value-based healthcare, it gives the companies an opportunity to have a conversation with their hospitals, because they are basically getting a free scrub tech or a free PA based on the amount of cases these high-performing sales reps see and the knowledge they have with ten to 20+ years in the OR. If [the hospital] doesn’t want to pay for that rep, they don’t have to. If they do want that rep there, it’s going to come with a different service model. That evolution will occur.”
Panelists did not dispute the value that sales reps bring to their companies and to the surgeon. As we have learned from previous conversations, industry sales leaders and consultants believe that the great sales reps will become more valuable as companies condense their forces. Additionally, while a portion of the market could be served under a repless model, companies would need to invest in technology and resources to ensure that outcomes are maintained.
Mr. Lohrer commented that removing the rep altogether would require foolproof technology, like a kit with one implant, minimal instrumentation, a technique guide and perhaps even a set staff to assist the surgeon. Keep an eye on the niche market of disposable or single-use systems currently found in spine and trauma.
Companies will take different approaches based on size, but there is an appetite at the hospital and device company level to play with salesforce dynamics.
Outpatient Procedures
The movement of procedures to ambulatory surgery centers (ASCs) is on the rise thanks to a number of factors, including the desire of payors and providers to decrease episode costs, and surgeons to maintain their autonomy in product preference. The increase in ASC procedures for spine, knee and hip—the three largest market segments, by our estimates—is in the hundreds of percents. The ASC could be a prime opportunity for small and medium-sized companies to compete.
Procedures performed in the outpatient setting are more predictable and require a smaller range of implants and instruments, Mr. Rose said. This could decrease the amount of capital spent on launching a new system, and could allow companies to scale faster and more efficiently.
“If [your company is] starting small, you don’t have a lot of revenue, a lot of infrastructure, a lot of reps, so I think it’s an opportunity to look at a problem in a different way,” Mr. Lohrer said. “In the U.S., Lima has a tiny market share. We’re pretty open. We’re not too worried about price levels. We know there are different kinds of customers, and we can think relatively freely about going to an ASC. Ten years ago, when I was a Synthes sales rep, that was not the case. I had the ASC, and then 200 yards away I had the hospital. I was worried about them finding out about each other’s different pricing levels. It’s a much more complicated relationship. For the small guys, it’s an opportunity to do what makes sense without worrying about what you’re losing.”
Reimbursement remains a challenge in the outpatient setting. Our conversations with spine and joint reconstruction surgeons in urban areas on both coasts have indicated that payors are beginning to incentivize surgeons who are able to demonstrate improved clinical and economic outcomes for ASC procedures. But work remains. For example, Medicare does not cover total hip or total joint procedures in the outpatient setting.
Mr. Rose reminded the audience that ASCs do require a higher level of service. There is often a closer relationship with sales reps and surgeons to ensure that the proper inventory is on hand, and there is an efficiency to surgeries that allows the ASC to turn over the operating room more quickly than in a hospital.
This observation from Mr. Rose aligns with our conversations with surgeons. For example, one ASC in particular requires two sets of instruments two days in advance of the surgery.
Additive Manufacturing
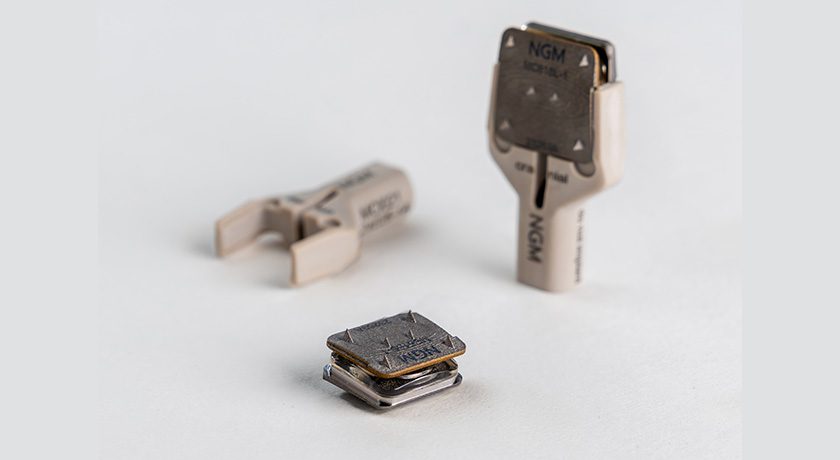
Orthopaedics’ adoption of additive manufacturing has created three groups: those that are fully invested and believe it can be revolutionary to the industry, those that have invested without a clear understanding of how the technology will ultimately be used, and those that are standing on the outside waiting for proof.
The consensus of the panel was that the technology’s benefits in device design, customization and bony ingrowth are proven. However, speed and cost remain large barriers to move the technology from niche to mainstream, and even then there was hesitation to say that it could be a player as a traditional manufacturing process by 2025.
Areas in which it could be helpful include customization for revisions or deformities, and even instrument manufacturing.
Dr. Bruder mentioned that Amendia 3D-prints instruments, which is a simpler process than printing devices. A surgeon can describe the length and dimensions of his preferred screwdriver, and the manufacturer can satisfy the surgeon in a way that doesn’t involve the complexity and liability of regulations associated with implants.
Incidentally, just hours before the panel convened, Stryker and GE—two of the larger players in additive—announced a materials, machine and supply chain partnership to support Stryker’s growth.
Mr. Rose, the most bullish of the bunch, pointed to ConforMIS’ and Stryker’s successes with additive products in total knee replacement.
“Recently, I heard an investor say, ‘Most people tend to overestimate change in the near term and underestimate change in the long term,’ ” he said. “It would be naïve to think that there’s not an opportunity to put a 3D printer in a hospital in ten or 15 years, and [device companies] can move some of the manufacturing closer to point of care. At the same time, I think we’re still very early in the stages of realizing what this technology is capable of in the long term, from a commercial standpoint.”
The panel discussed additional trends like robotics and episode-of-care solutions. Mr. Lohrer left the audience with the smart comment that in identifying trends and setting priorities, “You cannot lose track of growing your business.”
Carolyn LaWell is ORTHOWORLD’s Chief Content Officer. She can be reached by email.

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
CL
Carolyn LaWell is ORTHOWORLD's Chief Content Officer. She joined ORTHOWORLD in 2012 to oversee its editorial and industry education. She previously served in editor roles at B2B magazines and newspapers.