
 Copy to clipboard
Copy to clipboard 
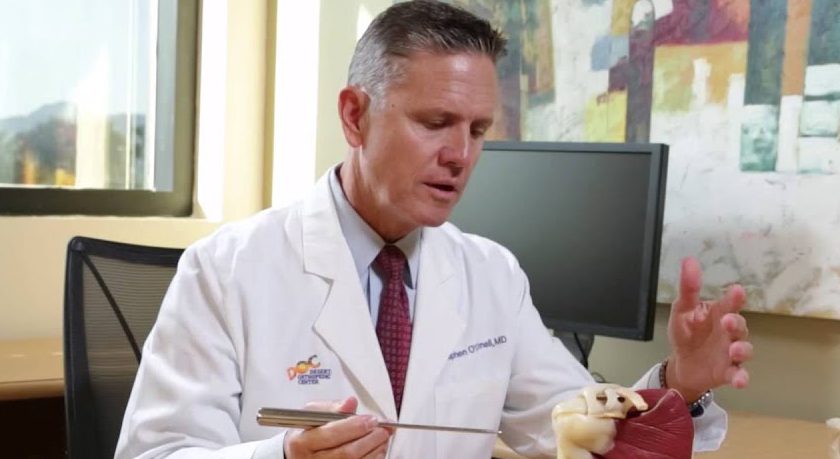
Some people are born to be surgeons. Others are natural-born leaders. Stephen J. O’Connell, M.D., happens to be both.
Dr. O’Connell, an upper-extremity orthopedic specialist, learned about the importance of taking care of employees during his childhood by watching his dad run local businesses. He’s fortunate to be able to bounce ideas off close friends who are CEOs of Fortune 500 companies.
Mostly, Dr. O’Connell learned to lead by running a private practice of 38 surgeons who co-manage the state-of-the-art Eisenhower Desert Orthopedic Center (EDOC), a hub of comprehensive care that’s affiliated with Eisenhower Health in Palm Springs, California.
“Around eight years ago, it was becoming more difficult to secure block times in Eisenhower Health’s main operating rooms due to increasing case volumes,” he said. “We recognized that a dedicated ASC for orthopedics would provide greater efficiency, cost-effectiveness, safety and improved outcomes.”
The ASC the physicians opened initially filled 55,000 square feet and included a clinic and two operating rooms. EDOC’s recent remodeling added 35,000 square feet and six operating rooms that are equipped with cutting-edge enabling technology, including six surgical robots. The one-stop-shop for orthopedic care includes an expanded clinic, occupational and physical therapy services, an imaging center and even a coffee shop.
It’s part of a grand vision that capitalizes on orthopedic surgery’s evolving landscape.
“We believe that adversarial relationships between hospitals and medical groups are counterproductive,” Dr. O’Connell said, “We opted for a collaborative approach as more complex cases shift to the outpatient setting. Aligning the incentives of our physicians and the health system drives cost-effective solutions that improve patient outcomes.”
Set Up for Same-day Surgery
The EDOC physicians anticipated a significant shift from inpatient to outpatient orthopedic care, and the data supports their assumption. In 2018, the average length of stay for their hip and knee replacement patients was 2.17 days and 2.27 days, respectively. By 2023, lengths of stay have decreased dramatically to 0.77 days for hips and 0.69 days for knees. Impressively, 80% of hip and knee replacement patients now leave the facility on the day of surgery.
“This transition over a relatively short period of time has been remarkable, particularly considering that 68% of our patients are Medicare recipients with an average age of 70,” Dr. O’Connell said.
Outpatient shoulder replacement surgery has experienced the most pronounced increase in volume over the last five years, according to Dr. O’Connell. Additionally, he said, fracture fixation and foot procedures have evolved and now include a broader range of equipment and innovative surgical approaches. This has led to a notable rise in the number of trauma and foot and ankle procedures performed in ASCs.
Dr. O’Connell and his colleagues remain focused on moving more procedures to the same-day setting. “We’re actively working on transitioning certain cervical spine surgeries and single-level lumbar procedures to our ASC,” Dr. O’Connell said. “This step signifies a broader trend toward maximizing the efficiency and benefits of outpatient care.”
Meeting the Needs of ASCs
Dr. O’Connell helped to establish a co-management committee at EDOC that has replaced the old practice of having individual doctors make decisions about which new technologies to add based on personal preferences or relationships with sales reps. This arrangement lacked accountability from the surgeon’s side and consequently made cost containment challenging.
The co-management committee — which comprises surgeons from EDOC and the head of central supply and the inpatient and outpatient operating rooms at Eisenhower Health — assesses new equipment and technologies. Surgeons who want to add devices must present the proposal to their colleagues and share outcomes data, pricing information and how the solution compares to existing options.
“This collaborative process ensures that we, as surgeons, are invested in maintaining cost-effective surgical care,” Dr. O’Connell said. “The approach has proven remarkably effective in aiding Eisenhower Health’s cost management efforts.”
One of the earliest projects brought to the co-management committee’s attention focused on surgical cement. After an extensive evaluation involving data analysis and discussions among the surgeons, the group reached a consensus and narrowed down six cement options to a single type that the surgeons agreed to use. This seemingly minor standardization amounted to nearly seven figures in annual savings.
“The committee has transformed our decision-making processes and allows our surgeon group to contribute actively to cost control efforts,” Dr. O’Connell said. “This collaborative approach fosters a more responsible and informed decision-making environment that generates value for patients. We strive to add equipment and technology that lead to improved outcomes while maintaining cost-effective care.”
Ultimately, the vendors that exhibit an understanding of the surgeons’ needs and concerns are most helpful and gain access to EDOC’s operating rooms. “Their ability to think like a surgeon, anticipate our requirements and align their solutions accordingly is a deciding factor in the companies with which we work,” Dr. O’Connell said.
Shared Incentives and Responsibilities
The ongoing transition to value-based care is a concern that keeps Dr. O’Connell awake at night.
“Balancing the delivery of high-quality outcomes with the pressures of increasing case volumes and patient expectations for rapid recoveries is challenging,” he said. “Navigating the complexities and financial interests of insurance companies and managed care organizations adds another layer of complexity. Advocating for patients’ best interests can be an uphill battle.”
The shifting of higher acuity patients and more intricate surgeries to outpatient facilities requires ASCs to be adequately equipped to manage complex cases, a factor that demands managing peripheral services and patient care requirements.
“With insurance companies decreasing their coverage for physical and occupational therapy, we’re entering an era in which virtual rehabilitation is gaining prominence,” Dr. O’Connell said. “Moving forward, physicians could invest more time in creating educational videos for patients, allowing them to revisit pre- and post-op instructions and exercise programs. This would foster better patient adherence to comprehensive treatment regimens.”
Collaborative ventures between hospitals and physicians, like the joint venture that runs EDOC, place decision-making authority in the hands of surgeons and align the incentives of multi-disciplinary teams involved in the continuum of care.
“The concept of shared responsibility for funds allocation encourages better decision-making,” Dr. O’Connell said. “When both parties share in the responsibilities and outcomes, it establishes a solid foundation for effective healthcare delivery.”
Inspiring the Next Generation of Leaders
Dr. O’Connell has always encouraged younger surgeons to take on administrative responsibilities and leadership roles.
“It’s important to usher in a new generation of surgeon leaders who are willing to invest their time and efforts in managing the concerns of the collective group and prioritizing them over their individual interests,” he said. “Grooming physicians to step into leadership roles, even if doing so doesn’t align with their personal preferences, is important for the continued growth of the profession.”
To further the cause, Dr. O’Connell always shares key advice that has served him well over the years.
“It’s crucial to embrace the notion that you won’t always achieve everything you desire individually,” he said. “Decisions are often reached through a group consensus and based on what’s best for the whole. Sometimes you win, and sometimes you don’t. However, collective growth invariably benefits everyone in the long run.”
Some people are born to be surgeons. Others are natural-born leaders. Stephen J. O’Connell, M.D., happens to be both.
Dr. O’Connell, an upper-extremity orthopedic specialist, learned about the importance of taking care of employees during his childhood by watching his dad run local businesses. He’s fortunate to be able to bounce ideas off...
Some people are born to be surgeons. Others are natural-born leaders. Stephen J. O’Connell, M.D., happens to be both.
Dr. O’Connell, an upper-extremity orthopedic specialist, learned about the importance of taking care of employees during his childhood by watching his dad run local businesses. He’s fortunate to be able to bounce ideas off close friends who are CEOs of Fortune 500 companies.
Mostly, Dr. O’Connell learned to lead by running a private practice of 38 surgeons who co-manage the state-of-the-art Eisenhower Desert Orthopedic Center (EDOC), a hub of comprehensive care that’s affiliated with Eisenhower Health in Palm Springs, California.
“Around eight years ago, it was becoming more difficult to secure block times in Eisenhower Health’s main operating rooms due to increasing case volumes,” he said. “We recognized that a dedicated ASC for orthopedics would provide greater efficiency, cost-effectiveness, safety and improved outcomes.”
The ASC the physicians opened initially filled 55,000 square feet and included a clinic and two operating rooms. EDOC’s recent remodeling added 35,000 square feet and six operating rooms that are equipped with cutting-edge enabling technology, including six surgical robots. The one-stop-shop for orthopedic care includes an expanded clinic, occupational and physical therapy services, an imaging center and even a coffee shop.
It’s part of a grand vision that capitalizes on orthopedic surgery’s evolving landscape.
“We believe that adversarial relationships between hospitals and medical groups are counterproductive,” Dr. O’Connell said, “We opted for a collaborative approach as more complex cases shift to the outpatient setting. Aligning the incentives of our physicians and the health system drives cost-effective solutions that improve patient outcomes.”
Set Up for Same-day Surgery
The EDOC physicians anticipated a significant shift from inpatient to outpatient orthopedic care, and the data supports their assumption. In 2018, the average length of stay for their hip and knee replacement patients was 2.17 days and 2.27 days, respectively. By 2023, lengths of stay have decreased dramatically to 0.77 days for hips and 0.69 days for knees. Impressively, 80% of hip and knee replacement patients now leave the facility on the day of surgery.
“This transition over a relatively short period of time has been remarkable, particularly considering that 68% of our patients are Medicare recipients with an average age of 70,” Dr. O’Connell said.
Outpatient shoulder replacement surgery has experienced the most pronounced increase in volume over the last five years, according to Dr. O’Connell. Additionally, he said, fracture fixation and foot procedures have evolved and now include a broader range of equipment and innovative surgical approaches. This has led to a notable rise in the number of trauma and foot and ankle procedures performed in ASCs.
Dr. O’Connell and his colleagues remain focused on moving more procedures to the same-day setting. “We’re actively working on transitioning certain cervical spine surgeries and single-level lumbar procedures to our ASC,” Dr. O’Connell said. “This step signifies a broader trend toward maximizing the efficiency and benefits of outpatient care.”
Meeting the Needs of ASCs
Dr. O’Connell helped to establish a co-management committee at EDOC that has replaced the old practice of having individual doctors make decisions about which new technologies to add based on personal preferences or relationships with sales reps. This arrangement lacked accountability from the surgeon’s side and consequently made cost containment challenging.
The co-management committee — which comprises surgeons from EDOC and the head of central supply and the inpatient and outpatient operating rooms at Eisenhower Health — assesses new equipment and technologies. Surgeons who want to add devices must present the proposal to their colleagues and share outcomes data, pricing information and how the solution compares to existing options.
“This collaborative process ensures that we, as surgeons, are invested in maintaining cost-effective surgical care,” Dr. O’Connell said. “The approach has proven remarkably effective in aiding Eisenhower Health’s cost management efforts.”
One of the earliest projects brought to the co-management committee’s attention focused on surgical cement. After an extensive evaluation involving data analysis and discussions among the surgeons, the group reached a consensus and narrowed down six cement options to a single type that the surgeons agreed to use. This seemingly minor standardization amounted to nearly seven figures in annual savings.
“The committee has transformed our decision-making processes and allows our surgeon group to contribute actively to cost control efforts,” Dr. O’Connell said. “This collaborative approach fosters a more responsible and informed decision-making environment that generates value for patients. We strive to add equipment and technology that lead to improved outcomes while maintaining cost-effective care.”
Ultimately, the vendors that exhibit an understanding of the surgeons’ needs and concerns are most helpful and gain access to EDOC’s operating rooms. “Their ability to think like a surgeon, anticipate our requirements and align their solutions accordingly is a deciding factor in the companies with which we work,” Dr. O’Connell said.
Shared Incentives and Responsibilities
The ongoing transition to value-based care is a concern that keeps Dr. O’Connell awake at night.
“Balancing the delivery of high-quality outcomes with the pressures of increasing case volumes and patient expectations for rapid recoveries is challenging,” he said. “Navigating the complexities and financial interests of insurance companies and managed care organizations adds another layer of complexity. Advocating for patients’ best interests can be an uphill battle.”
The shifting of higher acuity patients and more intricate surgeries to outpatient facilities requires ASCs to be adequately equipped to manage complex cases, a factor that demands managing peripheral services and patient care requirements.
“With insurance companies decreasing their coverage for physical and occupational therapy, we’re entering an era in which virtual rehabilitation is gaining prominence,” Dr. O’Connell said. “Moving forward, physicians could invest more time in creating educational videos for patients, allowing them to revisit pre- and post-op instructions and exercise programs. This would foster better patient adherence to comprehensive treatment regimens.”
Collaborative ventures between hospitals and physicians, like the joint venture that runs EDOC, place decision-making authority in the hands of surgeons and align the incentives of multi-disciplinary teams involved in the continuum of care.
“The concept of shared responsibility for funds allocation encourages better decision-making,” Dr. O’Connell said. “When both parties share in the responsibilities and outcomes, it establishes a solid foundation for effective healthcare delivery.”
Inspiring the Next Generation of Leaders
Dr. O’Connell has always encouraged younger surgeons to take on administrative responsibilities and leadership roles.
“It’s important to usher in a new generation of surgeon leaders who are willing to invest their time and efforts in managing the concerns of the collective group and prioritizing them over their individual interests,” he said. “Grooming physicians to step into leadership roles, even if doing so doesn’t align with their personal preferences, is important for the continued growth of the profession.”
To further the cause, Dr. O’Connell always shares key advice that has served him well over the years.
“It’s crucial to embrace the notion that you won’t always achieve everything you desire individually,” he said. “Decisions are often reached through a group consensus and based on what’s best for the whole. Sometimes you win, and sometimes you don’t. However, collective growth invariably benefits everyone in the long run.”

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
DC
Dan Cook is a senior editor with more than 18 years of experience in medical publishing and an extensive background in covering orthopedics and outpatient surgery. He joined ORTHOWORLD to develop content focused on important industry trends, top thought leaders and innovative technologies.







