
 Copy to clipboard
Copy to clipboard 
The purpose of this quarterly column is to introduce and discuss key considerations for device companies from the perspective of their customers: hospitals, health systems and physicians.
Value-based healthcare is a delivery model in which providers, including hospitals, physicians and other stakeholders, are paid based partially upon patient health outcomes. Value-based care contrasts with fee-for-service, in which providers are paid based on the amount of healthcare services they deliver and not necessarily the quality of care. As more of your hospital and surgeon customers embrace value-based healthcare, it is imperative to understand how you play a role in this reimbursement shift.
DEVICE COMPANIES SEEK TO UNDERSTAND VALUE-BASED CARE
As value-based healthcare, in its many forms, permeates delivery and reimbursement, the most immediate impact for device companies will be price pressure, forced downstream by risk holders (payors, hospitals, physicians, other providers) who must put together packaged healthcare services at a lower cost.
A specific example would be a hospital and surgeon joint replacement coalition contracting with a commercial payor for a full episode of care. The coalition will competitively position its package and seek price concessions from partners. Implants, a substantial cost for joint replacement, are an obvious target for cost reduction. In its simplest form, as more joint and spine care moves toward value-based reimbursement, device companies will need to offer strategic pricing levels to maintain business. A more complex version may require device companies to demonstrate that their products contribute to incrementally better outcomes over time. Exhibit 1 envisions not only the surgical event, but also a 12-month episode of care and quality considerations.
Exhibit 1: Surgical Event vs. Episode of Care

Joint replacement demand will continue to grow, with outpatient procedures steadily increasing. Even with increased payor scrutiny, spine surgery volumes are anticipated to grow overall, yet with an increasing percentage occurring in ambulatory surgical centers.
Many device companies have a strategic understanding of the impact of value-based care from their experience in joint replacement bundles with surgeons and hospitals. However, device companies may tactically choose to maintain a focus on the surgical event, growing market share and assuring pricing. If, however, device companies can demonstrate that their products favorably influence quality over a longer post-operative episode, customers may reconsider initial cost over time rather than just at implantation, which could result in price validation.
This quarterly column has consistently advocated for greater device company engagement with hospital executives and service line leadership as partners in cost and quality. Such a vendor-C-suite forum could be a basis and springboard for continued broader partnership.
We have again asked for expert opinions on “value.” These voices include:
- Joseph Tomaro, Ph.D., Consulting Director for Vizient
- Hassan Serhan, Ph.D., Adjunct Professor of Bioengineering, University of Toledo and Co-Founder & Treasurer of the International Musculoskeletal Society
- Marshall Steele, M.D., Founder and President Emeritus of Marshall Steele & Associates
- Dan Pizzarello, M.D., Founder and CEO of Risalto Health
ARE WE MEASURING THE RIGHT THINGS?
Joe Tomaro, Ph.D., Consulting Director, Vizient
While payors are gradually converting to value-based healthcare, the majority of today’s outcomes measures used for higher volume elective orthopedic procedures are focused on a small portion of the episode of care. Total joint replacement readmission rate is an example. Hospital readmission after joint replacement surgery is an important and sometimes costly issue. The U.S. national average is 4.2%, with only slight differences among hospitals. A recent review of CMS’s joint replacement readmission data suggests that this outcomes measure shows minimal recent improvement and may have reached its potential for improvement.
The emphasis over the past five years has been on a 90-day episode of care bundled payment model, mainly for total joints, but also hip fracture and spine—a step in the right direction for value-based healthcare in orthopedics. However, the focus of bundled payment programs remains cost improvement, with some outcomes improvement required for providers to share in savings. Most of these outcomes measures are early in the episode of care, such as hospital complications, readmission and hospital patient satisfaction. Additionally, some programs are collecting patient reported outcomes information on pain and function at three months as part of overall outcomes measures.
For many value-based orthopedic procedures (joint replacement, spine surgery and hip fracture repair), it has been shown repeatedly that patients do not reach their best outcome until at least six to nine months or even a full year after surgery. Therefore, perhaps the best way to measure value-based healthcare in orthopedics is by employing long-term measurements of patient reported outcomes. Long-term measurements will be challenging to implement, but they will be required if value-based healthcare payments remain predicated on a relative patient outcome.
SMART TECHNOLOGIES ADD VALUE
Hassan Serhan, Ph.D., Adjunct Professor of Bioengineering, University of Toledo and Co-Founder & Treasurer of the International Musculoskeletal Society
From his nearly 25 years of industry experience, Dr. Hassan Serhan offers unique insights on the future of medical devices and quality. Historically, device companies have focused on developing quality products for musculoskeletal conditions, yet have been distant from functional patient outcomes: less pain, greater mobility and function, return to work, improved quality of life, etc. According to Dr. Serhan, novel technologies could change that focus.
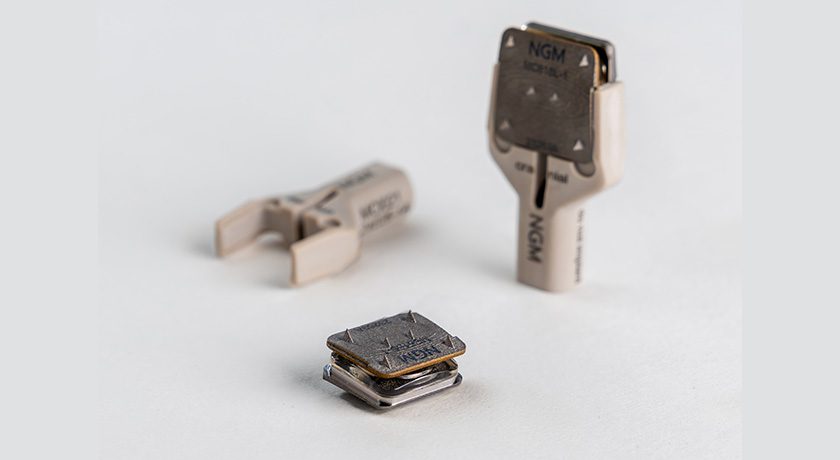
Sensing, Measuring and Advanced Reporting Technology (SMART) devices are creating a paradigm shift from episodic monitoring to continuous sensing and integrated healthcare. The emergence of SMART implants and instruments that transmit static and/or continuous feedback on implantables and surgical instruments could add value and affect quality. Smart instruments will lead to consistency in reproducible surgical procedures and may reduce intraoperative variabilities, which could alert surgeons to potential problems before a major complication occurs.
Dr. Serhan offered the example of Intellirod Spine’s transponder embedded in a spinal fusion implant to measure strain values intraoperatively, allowing surgeons to objectively assess the load on rods and potentially reduce failure rates. Intellirod is also in pursuit of an implantable sensor that measures strain value to predict fusion progression or excessive implant load. Several wearable and implantable devices are in development to allow the transmission of key biometric data, such as surgical site temperature relative to infection, strain or impedance to assess fusion rates, and patient activity levels relative to rehabilitation benchmarks. These quantitative data could be available to physicians or patients, as appropriate, and reported via wearable devices or monitoring software to manage care.
Additionally, experimental surgical instruments that verify proper surgical techniques are being tested to reduce surgical variability, ostensibly leading to better clinical outcomes. Zimmer Biomet’s iASSIST knee includes position sensors that determine alignment axes in relation to anatomical landmarks, and precisely position alignment instruments and implant components relative to these axes. Such technology innovations represent incremental additions to quality measurement as well as value over a longer post-operative period.
The current state of measuring and reporting patient functional outcomes through observation and use of survey tools such as Oswestry Disability Index and Neck Disability Index (spine), Hip Disability and Osteoarthritis Outcome Score and Knee Injury and Osteoarthritis Outcome Score (joint replacement) are standardized, but still subjective. However, the emergence of smart implants, wearables and smart instruments could generate that data to integrate with helpful but more subjective new clinical outcome standards to optimize both surgery and recovery.
STRATEGIC PRICE TRANSPARENCY WILL GROW
Marshall Steele, M.D., Marshall | Steele
Dr. Marshall Steele founded Marshall Steele & Associates in 1995 and served as President and Chief Executive Officer. Prior to founding his company, he held multiple roles—orthopedic surgeon, hospital medical director, author, entrepreneur and international consultant. In 2011, Stryker Orthopedics acquired Marshall | Steele, incorporating it into their Performance Solutions group. Dr. Steele is a widely-respected voice in orthopedics, business and medical leadership.
According to Dr. Steele, the healthcare industry is in dramatic transition. Patients have been largely left out of the purchasing process and cost considerations. Cost and quality initiatives are being fueled by employers and payors through strategies such as value-based care, risk-based contracting and population health. Dr. Steele asserts that device companies have not been substantially impacted by value-based care yet, but that time is coming. He anticipates that the future for device companies includes growing expectations for price transparency, tangible evidence of quality for buyers, continued downward price pressure and premium pricing only for truly differentiated products. Dr. Steele suggests that the primary near-term device company opportunity is strategic pricing that aligns with value-based care while seeking customer partnerships that support value well beyond surgery.
POPULATION HEALTH SPANS TOTAL EPISODE OF CARE
Dan Pizzarello, M.D., Founder and CEO, Risalto Health
Dr. Pizzarello saw an opportunity to address three critical opportunities in musculoskeletal services: access, quality and cost through a population health approach. Risalto’s model deploys big data to identify the best non-surgical and surgical providers, and supports them with expert care algorithms to offer a concierge model that delivers superior musculoskeletal care for patients. The model has found support among both employers and payors that seek solutions to high-cost, high utilization of spine, hip and knee services that cannot substantiate quality claims.
Like Dr. Steele and others, Dr. Pizzarello agrees that implant pricing will continue to face price pressure as reimbursement decreases, scrutiny of surgical spine increases and quality is measured. This pressure will take the structure of formulary pricing, vendor consolidation and other strategies.
SUMMARY
We thank our contributors for their unique insights. The mid- to long-term future will require increased evidence to support pricing and value by device companies. While one obvious answer may be price concessions, it can be contended that broader thinking and strategic response around quality might actually result in sustained and growing market share for OEMs, as well as greater value for customers—hospitals, physicians and patients.
The purpose of this quarterly column is to introduce and discuss key considerations for device companies from the perspective of their customers: hospitals, health systems and physicians.
Value-based healthcare is a delivery model in which providers, including hospitals, physicians and other stakeholders, are paid based partially upon patient...
The purpose of this quarterly column is to introduce and discuss key considerations for device companies from the perspective of their customers: hospitals, health systems and physicians.
Value-based healthcare is a delivery model in which providers, including hospitals, physicians and other stakeholders, are paid based partially upon patient health outcomes. Value-based care contrasts with fee-for-service, in which providers are paid based on the amount of healthcare services they deliver and not necessarily the quality of care. As more of your hospital and surgeon customers embrace value-based healthcare, it is imperative to understand how you play a role in this reimbursement shift.
DEVICE COMPANIES SEEK TO UNDERSTAND VALUE-BASED CARE
As value-based healthcare, in its many forms, permeates delivery and reimbursement, the most immediate impact for device companies will be price pressure, forced downstream by risk holders (payors, hospitals, physicians, other providers) who must put together packaged healthcare services at a lower cost.
A specific example would be a hospital and surgeon joint replacement coalition contracting with a commercial payor for a full episode of care. The coalition will competitively position its package and seek price concessions from partners. Implants, a substantial cost for joint replacement, are an obvious target for cost reduction. In its simplest form, as more joint and spine care moves toward value-based reimbursement, device companies will need to offer strategic pricing levels to maintain business. A more complex version may require device companies to demonstrate that their products contribute to incrementally better outcomes over time. Exhibit 1 envisions not only the surgical event, but also a 12-month episode of care and quality considerations.
Exhibit 1: Surgical Event vs. Episode of Care

Joint replacement demand will continue to grow, with outpatient procedures steadily increasing. Even with increased payor scrutiny, spine surgery volumes are anticipated to grow overall, yet with an increasing percentage occurring in ambulatory surgical centers.
Many device companies have a strategic understanding of the impact of value-based care from their experience in joint replacement bundles with surgeons and hospitals. However, device companies may tactically choose to maintain a focus on the surgical event, growing market share and assuring pricing. If, however, device companies can demonstrate that their products favorably influence quality over a longer post-operative episode, customers may reconsider initial cost over time rather than just at implantation, which could result in price validation.
This quarterly column has consistently advocated for greater device company engagement with hospital executives and service line leadership as partners in cost and quality. Such a vendor-C-suite forum could be a basis and springboard for continued broader partnership.
We have again asked for expert opinions on “value.” These voices include:
- Joseph Tomaro, Ph.D., Consulting Director for Vizient
- Hassan Serhan, Ph.D., Adjunct Professor of Bioengineering, University of Toledo and Co-Founder & Treasurer of the International Musculoskeletal Society
- Marshall Steele, M.D., Founder and President Emeritus of Marshall Steele & Associates
- Dan Pizzarello, M.D., Founder and CEO of Risalto Health
ARE WE MEASURING THE RIGHT THINGS?
Joe Tomaro, Ph.D., Consulting Director, Vizient
While payors are gradually converting to value-based healthcare, the majority of today’s outcomes measures used for higher volume elective orthopedic procedures are focused on a small portion of the episode of care. Total joint replacement readmission rate is an example. Hospital readmission after joint replacement surgery is an important and sometimes costly issue. The U.S. national average is 4.2%, with only slight differences among hospitals. A recent review of CMS’s joint replacement readmission data suggests that this outcomes measure shows minimal recent improvement and may have reached its potential for improvement.
The emphasis over the past five years has been on a 90-day episode of care bundled payment model, mainly for total joints, but also hip fracture and spine—a step in the right direction for value-based healthcare in orthopedics. However, the focus of bundled payment programs remains cost improvement, with some outcomes improvement required for providers to share in savings. Most of these outcomes measures are early in the episode of care, such as hospital complications, readmission and hospital patient satisfaction. Additionally, some programs are collecting patient reported outcomes information on pain and function at three months as part of overall outcomes measures.
For many value-based orthopedic procedures (joint replacement, spine surgery and hip fracture repair), it has been shown repeatedly that patients do not reach their best outcome until at least six to nine months or even a full year after surgery. Therefore, perhaps the best way to measure value-based healthcare in orthopedics is by employing long-term measurements of patient reported outcomes. Long-term measurements will be challenging to implement, but they will be required if value-based healthcare payments remain predicated on a relative patient outcome.
SMART TECHNOLOGIES ADD VALUE
Hassan Serhan, Ph.D., Adjunct Professor of Bioengineering, University of Toledo and Co-Founder & Treasurer of the International Musculoskeletal Society
From his nearly 25 years of industry experience, Dr. Hassan Serhan offers unique insights on the future of medical devices and quality. Historically, device companies have focused on developing quality products for musculoskeletal conditions, yet have been distant from functional patient outcomes: less pain, greater mobility and function, return to work, improved quality of life, etc. According to Dr. Serhan, novel technologies could change that focus.
Sensing, Measuring and Advanced Reporting Technology (SMART) devices are creating a paradigm shift from episodic monitoring to continuous sensing and integrated healthcare. The emergence of SMART implants and instruments that transmit static and/or continuous feedback on implantables and surgical instruments could add value and affect quality. Smart instruments will lead to consistency in reproducible surgical procedures and may reduce intraoperative variabilities, which could alert surgeons to potential problems before a major complication occurs.
Dr. Serhan offered the example of Intellirod Spine’s transponder embedded in a spinal fusion implant to measure strain values intraoperatively, allowing surgeons to objectively assess the load on rods and potentially reduce failure rates. Intellirod is also in pursuit of an implantable sensor that measures strain value to predict fusion progression or excessive implant load. Several wearable and implantable devices are in development to allow the transmission of key biometric data, such as surgical site temperature relative to infection, strain or impedance to assess fusion rates, and patient activity levels relative to rehabilitation benchmarks. These quantitative data could be available to physicians or patients, as appropriate, and reported via wearable devices or monitoring software to manage care.
Additionally, experimental surgical instruments that verify proper surgical techniques are being tested to reduce surgical variability, ostensibly leading to better clinical outcomes. Zimmer Biomet’s iASSIST knee includes position sensors that determine alignment axes in relation to anatomical landmarks, and precisely position alignment instruments and implant components relative to these axes. Such technology innovations represent incremental additions to quality measurement as well as value over a longer post-operative period.
The current state of measuring and reporting patient functional outcomes through observation and use of survey tools such as Oswestry Disability Index and Neck Disability Index (spine), Hip Disability and Osteoarthritis Outcome Score and Knee Injury and Osteoarthritis Outcome Score (joint replacement) are standardized, but still subjective. However, the emergence of smart implants, wearables and smart instruments could generate that data to integrate with helpful but more subjective new clinical outcome standards to optimize both surgery and recovery.
STRATEGIC PRICE TRANSPARENCY WILL GROW
Marshall Steele, M.D., Marshall | Steele
Dr. Marshall Steele founded Marshall Steele & Associates in 1995 and served as President and Chief Executive Officer. Prior to founding his company, he held multiple roles—orthopedic surgeon, hospital medical director, author, entrepreneur and international consultant. In 2011, Stryker Orthopedics acquired Marshall | Steele, incorporating it into their Performance Solutions group. Dr. Steele is a widely-respected voice in orthopedics, business and medical leadership.
According to Dr. Steele, the healthcare industry is in dramatic transition. Patients have been largely left out of the purchasing process and cost considerations. Cost and quality initiatives are being fueled by employers and payors through strategies such as value-based care, risk-based contracting and population health. Dr. Steele asserts that device companies have not been substantially impacted by value-based care yet, but that time is coming. He anticipates that the future for device companies includes growing expectations for price transparency, tangible evidence of quality for buyers, continued downward price pressure and premium pricing only for truly differentiated products. Dr. Steele suggests that the primary near-term device company opportunity is strategic pricing that aligns with value-based care while seeking customer partnerships that support value well beyond surgery.
POPULATION HEALTH SPANS TOTAL EPISODE OF CARE
Dan Pizzarello, M.D., Founder and CEO, Risalto Health
Dr. Pizzarello saw an opportunity to address three critical opportunities in musculoskeletal services: access, quality and cost through a population health approach. Risalto’s model deploys big data to identify the best non-surgical and surgical providers, and supports them with expert care algorithms to offer a concierge model that delivers superior musculoskeletal care for patients. The model has found support among both employers and payors that seek solutions to high-cost, high utilization of spine, hip and knee services that cannot substantiate quality claims.
Like Dr. Steele and others, Dr. Pizzarello agrees that implant pricing will continue to face price pressure as reimbursement decreases, scrutiny of surgical spine increases and quality is measured. This pressure will take the structure of formulary pricing, vendor consolidation and other strategies.
SUMMARY
We thank our contributors for their unique insights. The mid- to long-term future will require increased evidence to support pricing and value by device companies. While one obvious answer may be price concessions, it can be contended that broader thinking and strategic response around quality might actually result in sustained and growing market share for OEMs, as well as greater value for customers—hospitals, physicians and patients.

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
PV
Patrick Vega is Consulting Director for Vizient’s Excelerate and PPI Orthopedics. Mr. Vega consults to member hospitals, health systems and physicians in musculoskeletal services with a focus on high-value care by aligning cost, quality and performance.