Copy to clipboard
Copy to clipboard 
ORTHOWORLD handed out the inaugural OEM Awards at OMTEC 2025 and hosted a panel discussion with the winners, asking about catalysts and obstacles to innovation in today’s orthopedic industry. The honorees shared ways to get an idea to market and then gain surgeon adoption.
This year’s award winners included:
Enovis for Bold Leadership based on its cadence of product launches, strategic acquisitions and culture of growth.
Johnson & Johnson MedTech for Next-Gen Innovator for its build-to-buy strategy that led it to work with eCential Robotics to design and develop the VELYS Active Robotic-Assisted System.
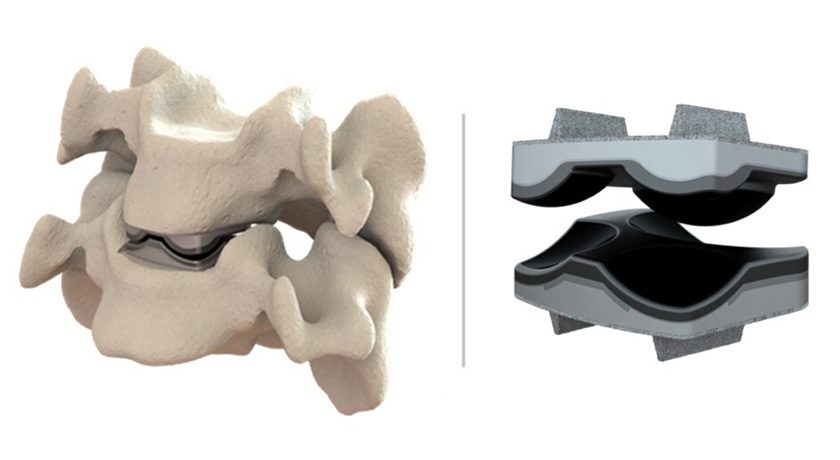
Foundational Surgical for Groundbreaking Device Design of their Vertiwedge Intraosseous Device, the first FDA-cleared, 3D-printed Class II spinal implant designed specifically for motion preservation.
Here, we provide edited highlights from the discussion to offer lessons learned and inspiration.
What are the Biggest Barriers to Innovation?
Asher Breverman, Foundation Surgical Director of Product and Marketing: The two biggest barriers for us are coding and reimbursement. Understanding the codes, how they’re used and why they’re important to a hospital or surgeon is critical to your organization. If you can’t get your device covered, no one is going to buy it.
The other challenge is regulatory. We have a Class II device, and the complexity of that landscape is that we’re being compared to AI-powered devices and smart implants. You have to understand how to navigate the regulatory pathway. The last thing you want is for FDA or an insurance company to come to you and say, ‘While you have a novel device, it doesn’t fit within our user needs or our metrics.’ You need to take a proactive approach and design your device with these constraints in mind.
Gary Justak, Enovis President and General Manager of Foot and Ankle: When we think about innovation, we account for price, site of care and the regulatory environment. We consider how to preserve the investment in NPI rather than get caught in a loop of constantly sustaining the products already on the market.
We took a pretty unique approach. When we undertook our six foot and ankle acquisitions, it was essential for us to preserve the R&D team from each of those sites. We also kept separate budgets for each of those sites so that we could manage innovation within each site and indication. We’ve really pushed the envelope on our thesis of focusing on differentiated technology. It’s important to preserve the innovation engine within your organization, regardless of size and scale, and focus your teams on driving new products that actually make a difference.
Bill Frasier, J&J MedTech Senior Technical Product Manager: Two hurdles come to mind for me. On the technical side, it’s the IP landscape. Many medical devices, electronics and technology companies have already claimed IP, and we have to find a way around it. We’re fortunate that, as a large company, we have many patent attorneys who help with the searches to find space to work.
The second hurdle is finding the resources and willingness to drive the product to market. Making a prototype of a unique product is hard in many ways. Once you get through that, you need to build your supply chain, commercial and training organization. It takes arguably as much or more to develop the technology as it does to get it to the market.
How do You Scale Innovation?
Justak: My advice is to fail fast. Ideation generation can come from anywhere in the organization. We have an intake process that encourages every employee or surgeon that we work with to submit ideas through an ideation process. We have skunk work teams that take ideation and turn it into a proof of concept that we could touch, feel and see if it has commercial viability. Having that control in place allows us to keep our key teams focused on the innovation that is already in scope and flight. Try anything within a construct, but don’t let ideas deter you from staying focused strategically.
Frasier: When you have a small team and a big idea, try to pull as much of that small team through as the team grows. It keeps the excitement and ownership level up, and the commitment can be infectious to the bigger team. As the project moves through the organization, it may get bogged down and start to lose its champion, so it’s important to have a core team that can drive the project all the way through to market.
Breverman: You need to know the clinical side better than everybody else. There’s a big difference between a widget with some form or function and a solution that solves an unmet clinical need. Understand the actual pain points of doctors by being in the operating room with them. Then, see how your device is used. Roll up your sleeves in the cadaver labs and put in the implant yourself. Those experiences spark true innovation.
There are numerous tools that you can use for rapid prototyping and team collaboration. Still, for me and our company, the real challenge has been understanding unmet clinical needs and figuring out how to solve them within the existing framework.
What’s Exciting about Today’s Advancements?
Breverman: We’re at a cool stage of innovation in the orthopedic industry, with artificial intelligence, smart implants, virtual reality headsets and the merging of hardware and software. We’re close to this bionic, transhumanist movement. Just look at Elon Musk and Neuralink.
People say this is the worst time to invest in or establish a startup. I think it’s the best time because you’ve never been able to do more with less. We’re seeing exponential growth in spine, and it’s exciting to finally see motion preservation and new technologies in spine finally catch on.
Justak: Enovis is doubling down on enabling technology. How do you empower or encourage a physician to do something different while giving them the feedback or insights that they need to be proficient in that surgery?
MIS is a perfect example. It’s a great benefit to the patient, but the learning curve is steep for physicians in foot and ankle. If you can create enabling technology that allows them to visualize and see things in real time, then you can really start to create a market.
Outside of enabling tech, one thing we’ve focused on since our inception is materials technology. We use nitinol to drive compressive dynamics post-surgery. We’re looking at different coatings and 3D printing. There are a lot of really unique things that we can do from a manufacturing perspective that will actually benefit the patient.
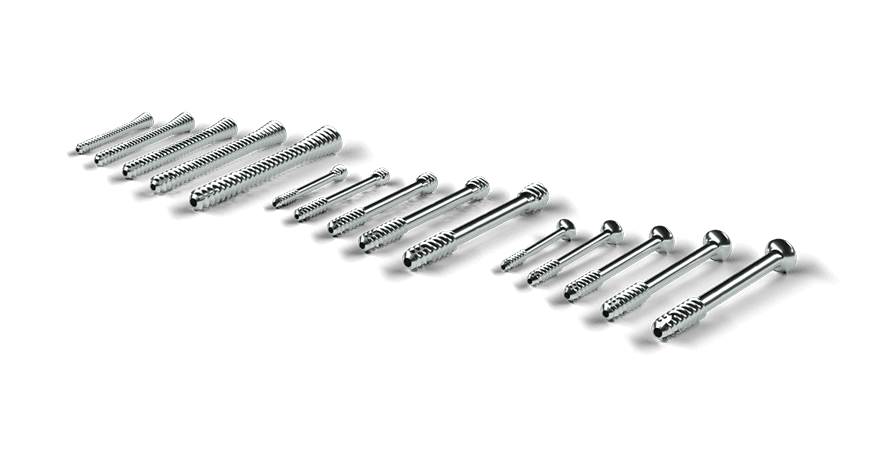
Frasier: We still don’t have the greatest outcomes in spine. Now that we’re deploying all of this technology, what do we do with the data we’re collecting? What is the right data to mine? How do we use the data to inform surgeons to do the right procedures for the right patients so that they get the best outcome? This means surgery is not based just on what the surgeon learned in their residency, the papers they’ve read, or the study groups they take part in. We can place pedicle screws and have great X-rays, but if the patient doesn’t have a great outcome, it doesn’t matter.
ORTHOWORLD handed out the inaugural OEM Awards at OMTEC 2025 and hosted a panel discussion with the winners, asking about catalysts and obstacles to innovation in today’s orthopedic industry. The honorees shared ways to get an idea to market and then gain surgeon adoption.
This year’s award winners included:
Enovis for Bold Leadership...
ORTHOWORLD handed out the inaugural OEM Awards at OMTEC 2025 and hosted a panel discussion with the winners, asking about catalysts and obstacles to innovation in today’s orthopedic industry. The honorees shared ways to get an idea to market and then gain surgeon adoption.
This year’s award winners included:
Enovis for Bold Leadership based on its cadence of product launches, strategic acquisitions and culture of growth.
Johnson & Johnson MedTech for Next-Gen Innovator for its build-to-buy strategy that led it to work with eCential Robotics to design and develop the VELYS Active Robotic-Assisted System.
Foundational Surgical for Groundbreaking Device Design of their Vertiwedge Intraosseous Device, the first FDA-cleared, 3D-printed Class II spinal implant designed specifically for motion preservation.
Here, we provide edited highlights from the discussion to offer lessons learned and inspiration.
What are the Biggest Barriers to Innovation?
Asher Breverman, Foundation Surgical Director of Product and Marketing: The two biggest barriers for us are coding and reimbursement. Understanding the codes, how they’re used and why they’re important to a hospital or surgeon is critical to your organization. If you can’t get your device covered, no one is going to buy it.
The other challenge is regulatory. We have a Class II device, and the complexity of that landscape is that we’re being compared to AI-powered devices and smart implants. You have to understand how to navigate the regulatory pathway. The last thing you want is for FDA or an insurance company to come to you and say, ‘While you have a novel device, it doesn’t fit within our user needs or our metrics.’ You need to take a proactive approach and design your device with these constraints in mind.
Gary Justak, Enovis President and General Manager of Foot and Ankle: When we think about innovation, we account for price, site of care and the regulatory environment. We consider how to preserve the investment in NPI rather than get caught in a loop of constantly sustaining the products already on the market.
We took a pretty unique approach. When we undertook our six foot and ankle acquisitions, it was essential for us to preserve the R&D team from each of those sites. We also kept separate budgets for each of those sites so that we could manage innovation within each site and indication. We’ve really pushed the envelope on our thesis of focusing on differentiated technology. It’s important to preserve the innovation engine within your organization, regardless of size and scale, and focus your teams on driving new products that actually make a difference.
Bill Frasier, J&J MedTech Senior Technical Product Manager: Two hurdles come to mind for me. On the technical side, it’s the IP landscape. Many medical devices, electronics and technology companies have already claimed IP, and we have to find a way around it. We’re fortunate that, as a large company, we have many patent attorneys who help with the searches to find space to work.
The second hurdle is finding the resources and willingness to drive the product to market. Making a prototype of a unique product is hard in many ways. Once you get through that, you need to build your supply chain, commercial and training organization. It takes arguably as much or more to develop the technology as it does to get it to the market.
How do You Scale Innovation?
Justak: My advice is to fail fast. Ideation generation can come from anywhere in the organization. We have an intake process that encourages every employee or surgeon that we work with to submit ideas through an ideation process. We have skunk work teams that take ideation and turn it into a proof of concept that we could touch, feel and see if it has commercial viability. Having that control in place allows us to keep our key teams focused on the innovation that is already in scope and flight. Try anything within a construct, but don’t let ideas deter you from staying focused strategically.
Frasier: When you have a small team and a big idea, try to pull as much of that small team through as the team grows. It keeps the excitement and ownership level up, and the commitment can be infectious to the bigger team. As the project moves through the organization, it may get bogged down and start to lose its champion, so it’s important to have a core team that can drive the project all the way through to market.
Breverman: You need to know the clinical side better than everybody else. There’s a big difference between a widget with some form or function and a solution that solves an unmet clinical need. Understand the actual pain points of doctors by being in the operating room with them. Then, see how your device is used. Roll up your sleeves in the cadaver labs and put in the implant yourself. Those experiences spark true innovation.
There are numerous tools that you can use for rapid prototyping and team collaboration. Still, for me and our company, the real challenge has been understanding unmet clinical needs and figuring out how to solve them within the existing framework.
What’s Exciting about Today’s Advancements?
Breverman: We’re at a cool stage of innovation in the orthopedic industry, with artificial intelligence, smart implants, virtual reality headsets and the merging of hardware and software. We’re close to this bionic, transhumanist movement. Just look at Elon Musk and Neuralink.
People say this is the worst time to invest in or establish a startup. I think it’s the best time because you’ve never been able to do more with less. We’re seeing exponential growth in spine, and it’s exciting to finally see motion preservation and new technologies in spine finally catch on.
Justak: Enovis is doubling down on enabling technology. How do you empower or encourage a physician to do something different while giving them the feedback or insights that they need to be proficient in that surgery?
MIS is a perfect example. It’s a great benefit to the patient, but the learning curve is steep for physicians in foot and ankle. If you can create enabling technology that allows them to visualize and see things in real time, then you can really start to create a market.
Outside of enabling tech, one thing we’ve focused on since our inception is materials technology. We use nitinol to drive compressive dynamics post-surgery. We’re looking at different coatings and 3D printing. There are a lot of really unique things that we can do from a manufacturing perspective that will actually benefit the patient.
Frasier: We still don’t have the greatest outcomes in spine. Now that we’re deploying all of this technology, what do we do with the data we’re collecting? What is the right data to mine? How do we use the data to inform surgeons to do the right procedures for the right patients so that they get the best outcome? This means surgery is not based just on what the surgeon learned in their residency, the papers they’ve read, or the study groups they take part in. We can place pedicle screws and have great X-rays, but if the patient doesn’t have a great outcome, it doesn’t matter.

You’ve reached your limit.
We’re glad you’re finding value in our content — and we’d love for you to keep going.
Subscribe now for unlimited access to orthopedic business intelligence.
CL
Carolyn LaWell is ORTHOWORLD's Chief Content Officer. She joined ORTHOWORLD in 2012 to oversee its editorial and industry education. She previously served in editor roles at B2B magazines and newspapers.