

 Copy to clipboard
Copy to clipboard 
In 2015, NASS conducted a survey taken by nearly 650 Members in the U.S. to support a clearer understanding of its Members’ practice settings. Please note: Of the respondents, roughly 70% (~455) were orthopaedic or neuro surgeons; another 19% were physicians, such as physical medicine and rehabilitation and anesthesiologist and 10% were non-physicians, such as chiropractors, physician assistants and physical/occupational therapists.
For years, studies have suggested that surgeons are fleeing private practice and aligning with hospitals. Respondents of this survey told a different story. When asked if their practice setting had changed in the past five to seven years, 81% said no, while 19% said yes.
More specifically, 64% said that they were employed by an independent group practice, a decrease of 4% from the previous five to seven years. Of respondents, 19% were employed by a hospital system, an increase of 3% from the previous five to seven years.
Regarding care models, changes in the past five to seven years were comparable with those of practice setting, with 81% of respondents saying that their care models hadn’t changed and 19% saying that they had.
 The most noticeable difference in care model changes came from those associated with accountable care organizations (ACOs). Of those who responded to the question, 23% said that they were now part of an ACO, an increase of 15% from the previous five to seven years. The second highest increase, about 4%, came from those now associated with Centers for Medicare & Medicaid Services’ (CMS) shared savings program and plans.
The most noticeable difference in care model changes came from those associated with accountable care organizations (ACOs). Of those who responded to the question, 23% said that they were now part of an ACO, an increase of 15% from the previous five to seven years. The second highest increase, about 4%, came from those now associated with Centers for Medicare & Medicaid Services’ (CMS) shared savings program and plans.
Spine could be a CMS target for mandatory alternative payment models in the future. However, the majority of survey respondents haven’t shifted resources in preparation for such an announcement. Of the respondents, 19% said that their healthcare delivery organization or practice has realigned resources in light of CMS’ call for increased alternative payments. The largest number of respondents—31%—said that they haven’t made changes, but plan to do so.
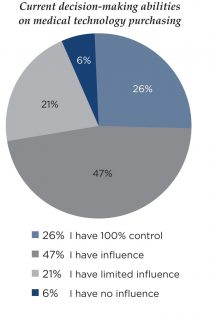
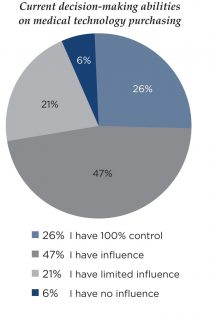
It is often discussed that surgeons have lost decision making power, which has been turned over to administrators. When asked about current decision-making abilities on medical technology purchasing, nearly 75% of respondents indicated that they have some or total influence on the matter.
Perhaps one lesson to take away from these results is that your customer isn’t stagnant. It’s wise to circle back from time to time and ask the same questions, because it’s likely that the answers will change or be different from the “popular” response or reported trend.
In 2015, NASS conducted a survey taken by nearly 650 Members in the U.S. to support a clearer understanding of its Members’ practice settings. Please note: Of the respondents, roughly 70% (55) were orthopaedic or neuro surgeons; another 19% were physicians, such as physical medicine and rehabilitation and anesthesiologist and 10% were...
In 2015, NASS conducted a survey taken by nearly 650 Members in the U.S. to support a clearer understanding of its Members’ practice settings. Please note: Of the respondents, roughly 70% (~455) were orthopaedic or neuro surgeons; another 19% were physicians, such as physical medicine and rehabilitation and anesthesiologist and 10% were non-physicians, such as chiropractors, physician assistants and physical/occupational therapists.
For years, studies have suggested that surgeons are fleeing private practice and aligning with hospitals. Respondents of this survey told a different story. When asked if their practice setting had changed in the past five to seven years, 81% said no, while 19% said yes.
More specifically, 64% said that they were employed by an independent group practice, a decrease of 4% from the previous five to seven years. Of respondents, 19% were employed by a hospital system, an increase of 3% from the previous five to seven years.
Regarding care models, changes in the past five to seven years were comparable with those of practice setting, with 81% of respondents saying that their care models hadn’t changed and 19% saying that they had.
 The most noticeable difference in care model changes came from those associated with accountable care organizations (ACOs). Of those who responded to the question, 23% said that they were now part of an ACO, an increase of 15% from the previous five to seven years. The second highest increase, about 4%, came from those now associated with Centers for Medicare & Medicaid Services’ (CMS) shared savings program and plans.
The most noticeable difference in care model changes came from those associated with accountable care organizations (ACOs). Of those who responded to the question, 23% said that they were now part of an ACO, an increase of 15% from the previous five to seven years. The second highest increase, about 4%, came from those now associated with Centers for Medicare & Medicaid Services’ (CMS) shared savings program and plans.
Spine could be a CMS target for mandatory alternative payment models in the future. However, the majority of survey respondents haven’t shifted resources in preparation for such an announcement. Of the respondents, 19% said that their healthcare delivery organization or practice has realigned resources in light of CMS’ call for increased alternative payments. The largest number of respondents—31%—said that they haven’t made changes, but plan to do so.
It is often discussed that surgeons have lost decision making power, which has been turned over to administrators. When asked about current decision-making abilities on medical technology purchasing, nearly 75% of respondents indicated that they have some or total influence on the matter.
Perhaps one lesson to take away from these results is that your customer isn’t stagnant. It’s wise to circle back from time to time and ask the same questions, because it’s likely that the answers will change or be different from the “popular” response or reported trend.

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
CL
Carolyn LaWell is ORTHOWORLD's Chief Content Officer. She joined ORTHOWORLD in 2012 to oversee its editorial and industry education. She previously served in editor roles at B2B magazines and newspapers.







