Copy to clipboard
Copy to clipboard 
This quarterly column on Hospital Trends will focus on the intersection of device manufacturers (also called vendors) and their provider customers (hospitals, health systems and physicians), offering perspective and insights directly from providers to device manufacturers. For providers, the combination of changes in reimbursement, physician employment and the ever-present drive to improve quality while reducing cost has resulted in an inflection point in the healthcare industry that has prompted device manufacturers and provider innovation to navigate uncharted waters.
While many manufacturers have endeavored to more effectively and strategically engage with customers, there is still great opportunity and challenge in doing so. For this column, I interviewed three thought-leading colleagues, asking, “What should device company/vendors consider when attempting to grow their business with providers?” I’ve also added my experience and insights gained from work in strategic assessment, planning and development in orthopedics and spine.
Panelists include:
- Kate Gillespie, R.N. BSN MBA, Assistant Vice President, Orthopaedics & Spine, Virtua Health, Marlton, New Jersey; President, New Jersey State Nurses Association, 2019
- Alok Sharan, M.D., MHCDS, Fellowship-trained Orthopedic Spine Surgeon; Co-Medical Director, WestMed Spine Center; Westchester, New York
- Fred Slunecka, 36 years with Avera Health, recently retired as Chief Operating Officer, Sioux Falls, South Dakota
Opportunity and Challenge
By intimately understanding provider customers and their product use cycle, device manufacturers can forge deeper relations that embed their products and themselves as preferred partners and ideally, expand the traditional supply boundaries and develop strategic partnerships with executive administration leadership.
Customers Are Changing; IDNs, Reimbursement, Supply Chain Processes
Across the country, hospitals, community-based services and practices have merged into multi-site, multi-service organizational entities over larger geographies, oftentimes called Integrated Delivery Networks (IDNs). This has resulted in strategic re-evaluation of service distribution within IDNs, and in some cases, the deployment, elimination or concentration of services at select locations. A manufacturer’s knowledge of this transforming provider environment is often limited beyond contact with typical touch points: physicians, purchasing and the supply chain. Understanding these developing realities can create strategic advantages for device manufacturers.
The strategic and tactical implications for manufacturers are several: increasingly centralized decision-making on purchasing, less influence among physicians due to more medical staff alignment with health systems, a heightened focus on demonstrable quality and the need to understand health systems beyond purchasing and supply chain.
Reimbursement
Although fee-for-service reimbursement is the dominant current model, payment is inexorably moving to models such as bundling, total-episode-of-care payment, capitation and other fixed-fee arrangements. This has required health systems to become fluent in and navigate new payment methodologies. While pay-for-performance can be financially rewarding, the learning curve is likely to increase the cost of business for providers. This fundamental shift should be understood by manufacturers, yet is often not.
What Do Hospitals/Health Systems Want Now?
In the constantly changing reimbursement environment, hospitals are scouring their organizations to reduce cost while improving quality. Current terms that describe these processes include value analysis, low-cost/high-value, process standardization, value-based reimbursement, vendor consolidation and physician/hospital partnerships.
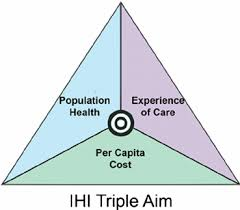
Additionally, the Institute for Healthcare Improvement (IHI) has pioneered a model for change, The “Triple Aim” that focuses on 1) improving clinical outcomes for populations, 2) reducing costs and 3) improving patient satisfaction as illustrated in the following graphic.
Exhibit 1: Institute for Healthcare Improvement’s Triple Aim
There is potentially a role for OEMs in this industry-wide initiative, not only delivering cost savings but also incremental service line benefits such as tools and insights to increase market share, redesign care, create differentiation and substantiate demonstrable quality. During the last 10 years, some OEMs have built or acquired “value-add” businesses with the intention of impacting hospital service lines beyond product and price. While providers have been open to such attempts, some value-add business units have devolved or been eliminated, ostensibly due to insufficient return on investment or a fundamental clash of internal cultures; sales versus service line redesign.
Think Outcomes, Expanded Sales Skills, Immersion
Alok Sharan, M.D., MHCDS, is Co-Director, WestMed Spine Center, and a practicing spine surgeon in Westchester, New York. He is also a pioneer in the Awake Spinal Fusion procedure, a novel outpatient surgical approach that does not require general anesthesia. Dr. Sharan’s observations include:
“First, as payment models move towards outcome-based reimbursement, vendors will need to be progressively aligned with physicians to get paid, in terms of quality of technology and implants, pricing and systems of care. Further, if vendors can demonstrate that their products contribute to better clinical and patient outcomes, they will be better positioned. Patient outcomes, sometimes referred to as ‘functional outcomes,’ go beyond surgical technique and implant to measure whether the patient actually gets better—less pain, more mobility, return to work, quality of life, etc. While not traditionally involved in functional outcomes, if vendors can link their products to improved functional outcomes, it could represent a significant differentiator that aligns with value-based reimbursement.
“Second, vendors have to expand the capabilities of their sales staff and re-envision the role they play to potentially include a greater awareness and conversance in the hospital and patient care environment. As previously noted, this could be a substantial challenge to the historical emphasis on selling to physician and supply chain.
“Third, vendors may want to consider immersing themselves in the clinic and with the physician environment to better understand patient and physician needs/preferences. Experience gained through immersion often yields surprising insights that span patient experience, physician preference, operational throughput and financial considerations.”
Think Beyond Cost to Strategic Partnerships, Understand Healthcare Systems
Fred Slunecka recently retired as Chief Operating Officer after 36 years with Avera Health. Mr. Slunecka now consults and advises health systems and OEMs with his tremendous depth of knowledge and credibility gained in the trenches of innovative hospital leadership. His comments reflect his personal observations and are not necessarily those of Avera.
“Strategic partnerships are likely to become more prevalent between suppliers and providers for a number of important reasons that include: 1) the growing size and sophistication of America’s largest health systems, including their development of integrated delivery networks; 2) payors’ insistence that providers take more risk in the provision of care for the duration of an illness or contract year (e.g. ACOs, capitation, etc.); 3) incredible pressures to reduce cost as payments dwindle and 4) better understanding by providers of what drives the overall cost of doing business.
“Hospitals are increasingly tasked to reduce supply costs and to commit volume and contracts in multi-year agreements. Examples may include long term agreements for CT scanners, PAC systems, chemistry analyzers, IV pumps, linear accelerators, drug dispensing systems, EMR, surgical mesh, contrast media, etc.
“As an IDN with organized clinical service lines, Avera was in a position to engage physicians like they have never been before. We told the clinical service lines that their prime job was to reduce the variation in care across Avera. Their job was to agree on specific vendors and equipment. Supply chain would negotiate with the selected vendors and bring all pricing information back to the physicians.
“This belief—reducing variation would drive cost reduction—has been overwhelmingly proven. As a side benefit, physician engagement has never been better. In one case, a low market share vendor for the system won a system-wide contract over a ‘product-only’ focused incumbent. This is just one example where, by taking initiative, vendors can solidify their relationships through ‘wearing the buyer’s hat’ and collaboratively crafting novel solutions.
“Moreover, the overall message was and is that suppliers who understand the challenges of providers and then design solutions for them will be the winners. Having the best box with the best juice was once all it took. Today, suppliers need to have a better understanding of how their equipment and services contribute to the overall improvement in care and reduction of cost. Suppliers need to understand how their systems drive the total cost of care. It is just that simple…and that hard.”
Advocate for the Customer, Leverage System Buying, Consider Transparent OEM Strategies
Kate Gillespie is Assistant Vice President for Orthopedics & Spine with Virtua Health, as well as recently elected President of the New Jersey State Nurses Association. Kate was among the leadership team that organized and launched a specialty hospital for joint replacement, the Virtua Joint Replacement Institute (VJRI), on their Voorhees campus. VJRI has achieved remarkable results in quality, growth and patient experience. Ms. Gillespie’s observations include:
In her experience, while vendors are often siloed by product, both vendor and hospital should be looking at the total organizational spend and service as they enter into negotiation. This will also allow both the vendor and hospital system to potentially capitalize on spend across various product and service lines. This could include implants, lighting, equipment, etc. A case in point was the purchase of three surgical robots, each with its own annual maintenance contract. With the robots being both within the Virtua system and geographically proximate to one another, it was mutually agreed for them to receive a discount on the annual maintenance fee.
Three years ago, some vendors seemed indifferent to Virtua’s underlying needs. With a strengthened vendor relations strategy and armed with market pricing data, the hospital has been able to approach the process with greater confidence. Their position is bolstered by formation of a spine/orthopedic product committee that meets with physicians in advance of vendor discussions and negotiations to precipitate and avoid triangulation between the vendor and physician. This reengineered process is illustrative of the impact of transparency setting the stage for more effective negotiations and relationship. An additional by-product of the relationship is the vendor’s knowledge and support of targeted cost reduction metrics for Virtua’s Clinically Integrated Network.
Final Thoughts
As hospitals, health systems and their associated provider environments become ever more complex, traditional approaches to establishing relationships, selling products and servicing accounts have become less effective. OEMs that endeavor to both understand the customer environment, in its full continuum, and meaningfully invest in a partnership with providers can be rewarded with market share growth, reciprocal value and more permanence in their relations with providers and IDNs.
To recap, OEMs should aspire to:
- Deeply understand hospital systems of care and the ways that their product “lives” in the provider and patient environments
- Seek a seat at the “strategy table” with hospital executive leadership
- Offer demonstrably differentiated products with data-supported outcomes
- Achieve conversance in all reimbursement models: fee for service, bundled payment, capitation and risk
- Pursue collaborative, long-term relationships with IDNs and physicians
This quarterly column on Hospital Trends will focus on the intersection of device manufacturers (also called vendors) and their provider customers (hospitals, health systems and physicians), offering perspective and insights directly from providers to device manufacturers. For providers, the combination of changes in reimbursement, physician...
This quarterly column on Hospital Trends will focus on the intersection of device manufacturers (also called vendors) and their provider customers (hospitals, health systems and physicians), offering perspective and insights directly from providers to device manufacturers. For providers, the combination of changes in reimbursement, physician employment and the ever-present drive to improve quality while reducing cost has resulted in an inflection point in the healthcare industry that has prompted device manufacturers and provider innovation to navigate uncharted waters.
While many manufacturers have endeavored to more effectively and strategically engage with customers, there is still great opportunity and challenge in doing so. For this column, I interviewed three thought-leading colleagues, asking, “What should device company/vendors consider when attempting to grow their business with providers?” I’ve also added my experience and insights gained from work in strategic assessment, planning and development in orthopedics and spine.
Panelists include:
- Kate Gillespie, R.N. BSN MBA, Assistant Vice President, Orthopaedics & Spine, Virtua Health, Marlton, New Jersey; President, New Jersey State Nurses Association, 2019
- Alok Sharan, M.D., MHCDS, Fellowship-trained Orthopedic Spine Surgeon; Co-Medical Director, WestMed Spine Center; Westchester, New York
- Fred Slunecka, 36 years with Avera Health, recently retired as Chief Operating Officer, Sioux Falls, South Dakota
Opportunity and Challenge
By intimately understanding provider customers and their product use cycle, device manufacturers can forge deeper relations that embed their products and themselves as preferred partners and ideally, expand the traditional supply boundaries and develop strategic partnerships with executive administration leadership.
Customers Are Changing; IDNs, Reimbursement, Supply Chain Processes
Across the country, hospitals, community-based services and practices have merged into multi-site, multi-service organizational entities over larger geographies, oftentimes called Integrated Delivery Networks (IDNs). This has resulted in strategic re-evaluation of service distribution within IDNs, and in some cases, the deployment, elimination or concentration of services at select locations. A manufacturer’s knowledge of this transforming provider environment is often limited beyond contact with typical touch points: physicians, purchasing and the supply chain. Understanding these developing realities can create strategic advantages for device manufacturers.
The strategic and tactical implications for manufacturers are several: increasingly centralized decision-making on purchasing, less influence among physicians due to more medical staff alignment with health systems, a heightened focus on demonstrable quality and the need to understand health systems beyond purchasing and supply chain.
Reimbursement
Although fee-for-service reimbursement is the dominant current model, payment is inexorably moving to models such as bundling, total-episode-of-care payment, capitation and other fixed-fee arrangements. This has required health systems to become fluent in and navigate new payment methodologies. While pay-for-performance can be financially rewarding, the learning curve is likely to increase the cost of business for providers. This fundamental shift should be understood by manufacturers, yet is often not.
What Do Hospitals/Health Systems Want Now?
In the constantly changing reimbursement environment, hospitals are scouring their organizations to reduce cost while improving quality. Current terms that describe these processes include value analysis, low-cost/high-value, process standardization, value-based reimbursement, vendor consolidation and physician/hospital partnerships.
Additionally, the Institute for Healthcare Improvement (IHI) has pioneered a model for change, The “Triple Aim” that focuses on 1) improving clinical outcomes for populations, 2) reducing costs and 3) improving patient satisfaction as illustrated in the following graphic.
Exhibit 1: Institute for Healthcare Improvement’s Triple Aim
There is potentially a role for OEMs in this industry-wide initiative, not only delivering cost savings but also incremental service line benefits such as tools and insights to increase market share, redesign care, create differentiation and substantiate demonstrable quality. During the last 10 years, some OEMs have built or acquired “value-add” businesses with the intention of impacting hospital service lines beyond product and price. While providers have been open to such attempts, some value-add business units have devolved or been eliminated, ostensibly due to insufficient return on investment or a fundamental clash of internal cultures; sales versus service line redesign.
Think Outcomes, Expanded Sales Skills, Immersion
Alok Sharan, M.D., MHCDS, is Co-Director, WestMed Spine Center, and a practicing spine surgeon in Westchester, New York. He is also a pioneer in the Awake Spinal Fusion procedure, a novel outpatient surgical approach that does not require general anesthesia. Dr. Sharan’s observations include:
“First, as payment models move towards outcome-based reimbursement, vendors will need to be progressively aligned with physicians to get paid, in terms of quality of technology and implants, pricing and systems of care. Further, if vendors can demonstrate that their products contribute to better clinical and patient outcomes, they will be better positioned. Patient outcomes, sometimes referred to as ‘functional outcomes,’ go beyond surgical technique and implant to measure whether the patient actually gets better—less pain, more mobility, return to work, quality of life, etc. While not traditionally involved in functional outcomes, if vendors can link their products to improved functional outcomes, it could represent a significant differentiator that aligns with value-based reimbursement.
“Second, vendors have to expand the capabilities of their sales staff and re-envision the role they play to potentially include a greater awareness and conversance in the hospital and patient care environment. As previously noted, this could be a substantial challenge to the historical emphasis on selling to physician and supply chain.
“Third, vendors may want to consider immersing themselves in the clinic and with the physician environment to better understand patient and physician needs/preferences. Experience gained through immersion often yields surprising insights that span patient experience, physician preference, operational throughput and financial considerations.”
Think Beyond Cost to Strategic Partnerships, Understand Healthcare Systems
Fred Slunecka recently retired as Chief Operating Officer after 36 years with Avera Health. Mr. Slunecka now consults and advises health systems and OEMs with his tremendous depth of knowledge and credibility gained in the trenches of innovative hospital leadership. His comments reflect his personal observations and are not necessarily those of Avera.
“Strategic partnerships are likely to become more prevalent between suppliers and providers for a number of important reasons that include: 1) the growing size and sophistication of America’s largest health systems, including their development of integrated delivery networks; 2) payors’ insistence that providers take more risk in the provision of care for the duration of an illness or contract year (e.g. ACOs, capitation, etc.); 3) incredible pressures to reduce cost as payments dwindle and 4) better understanding by providers of what drives the overall cost of doing business.
“Hospitals are increasingly tasked to reduce supply costs and to commit volume and contracts in multi-year agreements. Examples may include long term agreements for CT scanners, PAC systems, chemistry analyzers, IV pumps, linear accelerators, drug dispensing systems, EMR, surgical mesh, contrast media, etc.
“As an IDN with organized clinical service lines, Avera was in a position to engage physicians like they have never been before. We told the clinical service lines that their prime job was to reduce the variation in care across Avera. Their job was to agree on specific vendors and equipment. Supply chain would negotiate with the selected vendors and bring all pricing information back to the physicians.
“This belief—reducing variation would drive cost reduction—has been overwhelmingly proven. As a side benefit, physician engagement has never been better. In one case, a low market share vendor for the system won a system-wide contract over a ‘product-only’ focused incumbent. This is just one example where, by taking initiative, vendors can solidify their relationships through ‘wearing the buyer’s hat’ and collaboratively crafting novel solutions.
“Moreover, the overall message was and is that suppliers who understand the challenges of providers and then design solutions for them will be the winners. Having the best box with the best juice was once all it took. Today, suppliers need to have a better understanding of how their equipment and services contribute to the overall improvement in care and reduction of cost. Suppliers need to understand how their systems drive the total cost of care. It is just that simple…and that hard.”
Advocate for the Customer, Leverage System Buying, Consider Transparent OEM Strategies
Kate Gillespie is Assistant Vice President for Orthopedics & Spine with Virtua Health, as well as recently elected President of the New Jersey State Nurses Association. Kate was among the leadership team that organized and launched a specialty hospital for joint replacement, the Virtua Joint Replacement Institute (VJRI), on their Voorhees campus. VJRI has achieved remarkable results in quality, growth and patient experience. Ms. Gillespie’s observations include:
In her experience, while vendors are often siloed by product, both vendor and hospital should be looking at the total organizational spend and service as they enter into negotiation. This will also allow both the vendor and hospital system to potentially capitalize on spend across various product and service lines. This could include implants, lighting, equipment, etc. A case in point was the purchase of three surgical robots, each with its own annual maintenance contract. With the robots being both within the Virtua system and geographically proximate to one another, it was mutually agreed for them to receive a discount on the annual maintenance fee.
Three years ago, some vendors seemed indifferent to Virtua’s underlying needs. With a strengthened vendor relations strategy and armed with market pricing data, the hospital has been able to approach the process with greater confidence. Their position is bolstered by formation of a spine/orthopedic product committee that meets with physicians in advance of vendor discussions and negotiations to precipitate and avoid triangulation between the vendor and physician. This reengineered process is illustrative of the impact of transparency setting the stage for more effective negotiations and relationship. An additional by-product of the relationship is the vendor’s knowledge and support of targeted cost reduction metrics for Virtua’s Clinically Integrated Network.
Final Thoughts
As hospitals, health systems and their associated provider environments become ever more complex, traditional approaches to establishing relationships, selling products and servicing accounts have become less effective. OEMs that endeavor to both understand the customer environment, in its full continuum, and meaningfully invest in a partnership with providers can be rewarded with market share growth, reciprocal value and more permanence in their relations with providers and IDNs.
To recap, OEMs should aspire to:
- Deeply understand hospital systems of care and the ways that their product “lives” in the provider and patient environments
- Seek a seat at the “strategy table” with hospital executive leadership
- Offer demonstrably differentiated products with data-supported outcomes
- Achieve conversance in all reimbursement models: fee for service, bundled payment, capitation and risk
- Pursue collaborative, long-term relationships with IDNs and physicians

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
PV
Patrick Vega is Consulting Director for Vizient’s Excelerate and PPI Orthopedics. Mr. Vega consults to member hospitals, health systems and physicians in musculoskeletal services with a focus on high-value care by aligning cost, quality and performance.