Copy to clipboard
Copy to clipboard 
Preview
The purpose of this article and quarterly column is to introduce and discuss key considerations for vendors from the perspective of providers: hospitals, health systems and physicians. This Q3 column will provide a summary of ambulatory settings and strategies as they have been impacted by the pandemic.
COVID-19 has wrought remarkable changes to healthcare and across the spectrum of all care settings. Specifically, the virus has fueled and accelerated the movement of orthopedic and spine cases from traditional inpatient settings to ambulatory settings. Forward-thinking orthopedic vendors, or orthopedic companies, will invest both strategic and tactical resources to understand, predict and capitalize on these changes. We have engaged several experts to share their unique perspectives as well as make suggestions for vendors on how to leverage this shift.
Situation
The historical orthopedic model has been inpatient focused, with high revenue, high margin requiring extensive infrastructure and resources. The emerging model is both inpatient and ambulatory. The principal reasons for this shift include the following:
- Patient preference for a least restrictive level of care coupled with the convenience of proximate and community-based care
- First-time or enhanced reimbursement for ambulatory-based procedures, which might include such specific models as bundled payment or site-neutral reimbursement
- Improved technology and patient safety: these include pain management techniques, ambulatory patient care pathways, minimally invasive surgical techniques, patient selection and highly defined treatment protocols
- Specific to COVID-19, drivers of change may include unavailable/reduced inpatient surgical block time, longer waits for elective inpatient surgery, patient fear and avoidance of hospital settings, broader patient inclusion/selection criteria, and preservation/restoration of surgical revenue for physicians
ASC Trends
Hospitals can expect that surgeons will continue to take clinically appropriate patients to the ambulatory setting, resulting in a net loss of inpatient volume. Further, the percentage of ambulatory cases will not remain static; rather, the numbers will grow. Many hospitals and health systems are ill-prepared to capitalize on the ambulatory opportunity. Their challenge lies in that if they have not committed strategically and tactically to proactively move cases, they are at risk for ambulatory surgery centers (ASCs), which are often physician-owned, to more rapidly gear up and take market share.
In simple terms, hospitals risk losing a substantial number of these cases to more focused and better-prepared physician competitors. Proactive vendors and health systems should be devoting strategic and tactical resources to leverage the market reality rather than lag among competitors.
Where does Surgery Occur?
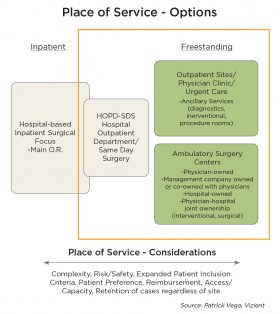
The graphic in Exhibit 1 illustrates both place of service options and considerations for selecting a place of care. The continuum of options includes hospital inpatient and hospital outpatient departments, the latter of which may be a dedicated same-day surgical suite or department or simply the use of the main operating room suites for same-day cases. ASCs are typically specialty focused such as orthopedics, spine, ENT, interventional pain management and others.
Some specific callouts for the graphic:
- The orange box encompasses all ambulatory options
- The four ownership models listed in ASC settings may each dictate different strategies
- For the hospital/health system, “retention” of cases within their spectrum of sites, whether inpatient or outpatient, will become imperative
Orthopedic Company Considerations
Traditionally, orthopedic vendors have seen the surgeon, purchasing and supply chain as their principal customer contacts. More broadly, with the emergence of integrated delivery networks and the supply chain having more visibility as a strategic department, such as a corporate or regional supply chain entity, decision makers have increased in numbers and scope of influence. From a vendor perspective, this requires additional skill sets beyond that of supporting the surgeon in the operating room. These additional skills require an expanded knowledge of and relationship with all points of care — inpatient, hospital outpatient department, outpatient sites, ASCs — as well as their cost containment strategies and how their products are used in patient care.
Panel of Experts
We solicited insights, opinion and expertise from a number of professionals across hospitals, vendors, medical staff and consultants with experience in ambulatory care. Each brings a unique understanding of the opportunities and challenges of capturing and leveraging the burgeoning growth of ambulatory care. Panelists’ perspectives may speak directly to vendor opportunity or may describe a system of care within which proactive vendors can explore and innovate.
Ryota Terada – Director, Orthopedics Intelligence &
Payment and Policy, Sg2
Kate Zentner – Director, Neurosciences, Sg2
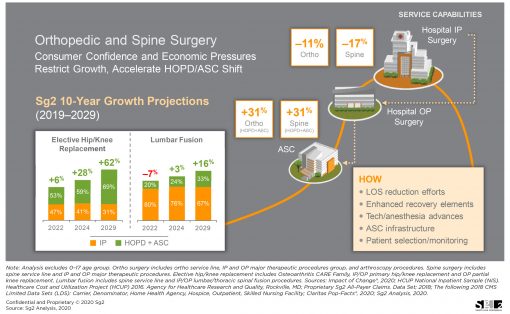
Among hospitals and health systems, the shift of inpatient cases to outpatient status and to ASCs has been top of mind since CMS removed total knee arthroplasty from the inpatient only list from 2018 and subsequently approved ASC payment for 2020. The initial severe, and now lingering, limitations imposed by COVID-19 have driven wider adoption of outpatient and ambulatory service options. Zentner and Terada shared the graphic in Exhibit 2 that projects a strong 10-year growth in ambulatory procedures and declines in inpatient hospital-based settings, along with the rationale for the transition. Sg2 predicts that orthopedic and spine procedures will grow +31% in ambulatory settings and will decrease -11% for orthopedics and -17% for spine in the inpatient setting.
Based on their deep market, provider and data knowledge, the rate of shift to ASC settings is very market specific and requires a hyper-localized analysis. These market factors impacting shift include physician ownership of ASCs, physician comfort with patient selection criteria, state regulatory climate for ASCs, consumer demand or reticence for care in the ASC setting, and pressure from payors and employers. These factors may act as a brake or an accelerator for a given market. For example, Zentner and Terada have seen markets where commercial payors may actually hinder the shift, whereas others may implement policies that promote aggressive shifts – even imposing site of care restrictions favoring ASCs to do so. The interplay between these brakes and accelerators will be critical for gauging the potential and rate of shift to the ASC setting at the market level.
Brian Asmussen – Director, Business Development & Strategy Healthcare Economics, Policy, & Reimbursement
Medtronic – Spine & Biologics | Restorative Therapies Group
While always a consideration for Medtronic, there is a renewed focus on the ambulatory market driven by projected growth, interrupted and diminished inpatient O.R. capacity, and avoidance of hospital settings in the current environment. The company has engaged customers across the full care continuum to continue to learn and hear from them about their unique needs in different sites of care. Medtronic is attentive to opportunities to address the specific needs of the ASC, including patient safety, procedural efficiency, value-based products, smaller facility footprint, less storage and sterile processing capacity. Relative to the ambulatory setting, Asmussen sees stakeholders such as hospitals, physicians, management companies and private equity all aligning in alternative sites of care well positioned for continued growth.
Ernie Robles – Consulting Director, Musculoskeletal
Service Lines, Vizient
Robles’ 10-year background in ambulatory care informs his perspective that there is opportunity for vendors to support providers through strategic pricing and terms for ASC-specific products and services. Commitment rebates, consigned inventory and bundled product pricing are a few favorable strategies that vendors can offer to differentiate from competitors. Furthermore, vendors might assist providers by offering more favorable payment terms as the organizations emerge from decreased cash flow caused by slow-downs or shut-downs. Additionally, business support might include physician recruitment and operational support in ASCs, adding new procedure types.
Chris Bishop – Chief Executive Officer,
Regent Surgical Health
As partners, consultants and advisors to the ASC space, much of Bishop’s focus lies in executing marketing strategies for Regent’s long-term growth strategy, as well as roll out of new outpatient service lines. Bishop believes that value propositions for the ambulatory space have changed as COVID has emerged. Traditional drivers of ASC growth remain constant — specialization/focused care, quality, decreased cost, efficiency, specialized staff and lower fixed costs. However, COVID has created opportunistic growth and incremental volume for ASCs that can anticipate impacts and nimbly respond. Paradoxically, as COVID may bring welcomed new volume, it can initially still be destabilizing operationally and clinically.
During COVID, Regent has seen increased volumes, new higher acuity joint patients through expansion of inclusion criteria, and older patients with more comorbidities. Regent returned to 90% of budgeted cases in June. A large percentage of those cases have been driven by patient preference to have procedures done sooner as an outpatient, rather than later as an inpatient.
Bishop also observes some potential opportunities for COVID-stressed ASCs:
- Consider converting ASCs to COVID treatment facilities
- Develop and implement more precise preoperative templating that increases accuracy and surgical preparedness (fewer trial sizes and implant options), thus less costly
- Consider lower price products and strive to be less brand sensitive
Increase focus on utilization and efficiency; fewer trays equate to less cost and the cumulative value of decreased case time - Create strategic partnerships between vendors and ASCs. There are physician ASC owners who don’t want to partner with private equity or get purchased by health systems and may be receptive to specific or broad consulting from vendors for operational, clinical and practice elements such as billing and collections.
Takeaways for Orthopedic Companies
There are several general advisements for orthopedic vendors seeking to expand or enter the ambulatory setting.
- Continuing price pressure driven by specialty hospitals with ambulatory services, often with physician ownership. Ambulatory providers will pursue preferential implant pricing to drive improved margins as well as to competitively price their services for such reimbursement models as bundled payment.
- Presumably, vendors are interested in maintaining their surgeon’s loyalty for products not only for the inpatient setting but for the outpatient setting as well. Vendors will be wise to address and support the delicate balance that surgeons must maintain between their inpatient hospital-based interests and their ambulatory interests relative to place of surgery and implant selection.
- Assess current levels of outpatient and ambulatory business relative to product sales; stand up resources to understand, plan and execute an ambulatory strategy.
- Evaluate whether inpatient products and services can be applied to the ambulatory setting or if new or modified products are required.
- Evaluate whether the sports medicine model of sales and service is an applicable model for joints and spine.
- Understand whether there is an opportunity to support and collaborate in the development of ambulatory protocols for joints and spine, patient oriented applications, pre-surgical patient education, site-specific instrument tray configurations, novel techniques and processes.
- When an ASC is physician-owned, there is potentially a substantial “first-mover advantage” for vendors that intentionally develop and execute an ambulatory strategy, because owners tend to be more price sensitive and less brand sensitive, but this too is likely to concretize over time.
Summary of Comments
COVID-19 will be an enduring guest in our healthcare environment; its impact likely vacillating between acute and chronic. Despite this, there is both need and opportunity for a dedicated ambulatory strategy for vendors. As vendors’ customers, whether physicians or hospitals, intentionally move cases to ambulatory settings, vendor services and strategies will need retooling. Essentially, vendors will need to more effectively “sync” with their ambulatory customers for product, service and strategy. It is a certainty that volumes will move, perhaps rapidly. For all stakeholders, a critical question looms, in the face of COVID: will they be proactive and realize the benefits, or reactive and become less competitive?
Preview
The purpose of this article and quarterly column is to introduce and discuss key considerations for vendors from the perspective of providers: hospitals, health systems and physicians. This Q3 column will provide a summary of ambulatory settings and strategies as they have been impacted by the pandemic.
COVID-19 has wrought remarkable...
Preview
The purpose of this article and quarterly column is to introduce and discuss key considerations for vendors from the perspective of providers: hospitals, health systems and physicians. This Q3 column will provide a summary of ambulatory settings and strategies as they have been impacted by the pandemic.
COVID-19 has wrought remarkable changes to healthcare and across the spectrum of all care settings. Specifically, the virus has fueled and accelerated the movement of orthopedic and spine cases from traditional inpatient settings to ambulatory settings. Forward-thinking orthopedic vendors, or orthopedic companies, will invest both strategic and tactical resources to understand, predict and capitalize on these changes. We have engaged several experts to share their unique perspectives as well as make suggestions for vendors on how to leverage this shift.
Situation
The historical orthopedic model has been inpatient focused, with high revenue, high margin requiring extensive infrastructure and resources. The emerging model is both inpatient and ambulatory. The principal reasons for this shift include the following:
- Patient preference for a least restrictive level of care coupled with the convenience of proximate and community-based care
- First-time or enhanced reimbursement for ambulatory-based procedures, which might include such specific models as bundled payment or site-neutral reimbursement
- Improved technology and patient safety: these include pain management techniques, ambulatory patient care pathways, minimally invasive surgical techniques, patient selection and highly defined treatment protocols
- Specific to COVID-19, drivers of change may include unavailable/reduced inpatient surgical block time, longer waits for elective inpatient surgery, patient fear and avoidance of hospital settings, broader patient inclusion/selection criteria, and preservation/restoration of surgical revenue for physicians
ASC Trends
Hospitals can expect that surgeons will continue to take clinically appropriate patients to the ambulatory setting, resulting in a net loss of inpatient volume. Further, the percentage of ambulatory cases will not remain static; rather, the numbers will grow. Many hospitals and health systems are ill-prepared to capitalize on the ambulatory opportunity. Their challenge lies in that if they have not committed strategically and tactically to proactively move cases, they are at risk for ambulatory surgery centers (ASCs), which are often physician-owned, to more rapidly gear up and take market share.
In simple terms, hospitals risk losing a substantial number of these cases to more focused and better-prepared physician competitors. Proactive vendors and health systems should be devoting strategic and tactical resources to leverage the market reality rather than lag among competitors.
Where does Surgery Occur?
The graphic in Exhibit 1 illustrates both place of service options and considerations for selecting a place of care. The continuum of options includes hospital inpatient and hospital outpatient departments, the latter of which may be a dedicated same-day surgical suite or department or simply the use of the main operating room suites for same-day cases. ASCs are typically specialty focused such as orthopedics, spine, ENT, interventional pain management and others.
Some specific callouts for the graphic:
- The orange box encompasses all ambulatory options
- The four ownership models listed in ASC settings may each dictate different strategies
- For the hospital/health system, “retention” of cases within their spectrum of sites, whether inpatient or outpatient, will become imperative
Orthopedic Company Considerations
Traditionally, orthopedic vendors have seen the surgeon, purchasing and supply chain as their principal customer contacts. More broadly, with the emergence of integrated delivery networks and the supply chain having more visibility as a strategic department, such as a corporate or regional supply chain entity, decision makers have increased in numbers and scope of influence. From a vendor perspective, this requires additional skill sets beyond that of supporting the surgeon in the operating room. These additional skills require an expanded knowledge of and relationship with all points of care — inpatient, hospital outpatient department, outpatient sites, ASCs — as well as their cost containment strategies and how their products are used in patient care.
Panel of Experts
We solicited insights, opinion and expertise from a number of professionals across hospitals, vendors, medical staff and consultants with experience in ambulatory care. Each brings a unique understanding of the opportunities and challenges of capturing and leveraging the burgeoning growth of ambulatory care. Panelists’ perspectives may speak directly to vendor opportunity or may describe a system of care within which proactive vendors can explore and innovate.
Ryota Terada – Director, Orthopedics Intelligence &
Payment and Policy, Sg2
Kate Zentner – Director, Neurosciences, Sg2
Among hospitals and health systems, the shift of inpatient cases to outpatient status and to ASCs has been top of mind since CMS removed total knee arthroplasty from the inpatient only list from 2018 and subsequently approved ASC payment for 2020. The initial severe, and now lingering, limitations imposed by COVID-19 have driven wider adoption of outpatient and ambulatory service options. Zentner and Terada shared the graphic in Exhibit 2 that projects a strong 10-year growth in ambulatory procedures and declines in inpatient hospital-based settings, along with the rationale for the transition. Sg2 predicts that orthopedic and spine procedures will grow +31% in ambulatory settings and will decrease -11% for orthopedics and -17% for spine in the inpatient setting.
Based on their deep market, provider and data knowledge, the rate of shift to ASC settings is very market specific and requires a hyper-localized analysis. These market factors impacting shift include physician ownership of ASCs, physician comfort with patient selection criteria, state regulatory climate for ASCs, consumer demand or reticence for care in the ASC setting, and pressure from payors and employers. These factors may act as a brake or an accelerator for a given market. For example, Zentner and Terada have seen markets where commercial payors may actually hinder the shift, whereas others may implement policies that promote aggressive shifts – even imposing site of care restrictions favoring ASCs to do so. The interplay between these brakes and accelerators will be critical for gauging the potential and rate of shift to the ASC setting at the market level.
Brian Asmussen – Director, Business Development & Strategy Healthcare Economics, Policy, & Reimbursement
Medtronic – Spine & Biologics | Restorative Therapies Group
While always a consideration for Medtronic, there is a renewed focus on the ambulatory market driven by projected growth, interrupted and diminished inpatient O.R. capacity, and avoidance of hospital settings in the current environment. The company has engaged customers across the full care continuum to continue to learn and hear from them about their unique needs in different sites of care. Medtronic is attentive to opportunities to address the specific needs of the ASC, including patient safety, procedural efficiency, value-based products, smaller facility footprint, less storage and sterile processing capacity. Relative to the ambulatory setting, Asmussen sees stakeholders such as hospitals, physicians, management companies and private equity all aligning in alternative sites of care well positioned for continued growth.
Ernie Robles – Consulting Director, Musculoskeletal
Service Lines, Vizient
Robles’ 10-year background in ambulatory care informs his perspective that there is opportunity for vendors to support providers through strategic pricing and terms for ASC-specific products and services. Commitment rebates, consigned inventory and bundled product pricing are a few favorable strategies that vendors can offer to differentiate from competitors. Furthermore, vendors might assist providers by offering more favorable payment terms as the organizations emerge from decreased cash flow caused by slow-downs or shut-downs. Additionally, business support might include physician recruitment and operational support in ASCs, adding new procedure types.
Chris Bishop – Chief Executive Officer,
Regent Surgical Health
As partners, consultants and advisors to the ASC space, much of Bishop’s focus lies in executing marketing strategies for Regent’s long-term growth strategy, as well as roll out of new outpatient service lines. Bishop believes that value propositions for the ambulatory space have changed as COVID has emerged. Traditional drivers of ASC growth remain constant — specialization/focused care, quality, decreased cost, efficiency, specialized staff and lower fixed costs. However, COVID has created opportunistic growth and incremental volume for ASCs that can anticipate impacts and nimbly respond. Paradoxically, as COVID may bring welcomed new volume, it can initially still be destabilizing operationally and clinically.
During COVID, Regent has seen increased volumes, new higher acuity joint patients through expansion of inclusion criteria, and older patients with more comorbidities. Regent returned to 90% of budgeted cases in June. A large percentage of those cases have been driven by patient preference to have procedures done sooner as an outpatient, rather than later as an inpatient.
Bishop also observes some potential opportunities for COVID-stressed ASCs:
- Consider converting ASCs to COVID treatment facilities
- Develop and implement more precise preoperative templating that increases accuracy and surgical preparedness (fewer trial sizes and implant options), thus less costly
- Consider lower price products and strive to be less brand sensitive
Increase focus on utilization and efficiency; fewer trays equate to less cost and the cumulative value of decreased case time - Create strategic partnerships between vendors and ASCs. There are physician ASC owners who don’t want to partner with private equity or get purchased by health systems and may be receptive to specific or broad consulting from vendors for operational, clinical and practice elements such as billing and collections.
Takeaways for Orthopedic Companies
There are several general advisements for orthopedic vendors seeking to expand or enter the ambulatory setting.
- Continuing price pressure driven by specialty hospitals with ambulatory services, often with physician ownership. Ambulatory providers will pursue preferential implant pricing to drive improved margins as well as to competitively price their services for such reimbursement models as bundled payment.
- Presumably, vendors are interested in maintaining their surgeon’s loyalty for products not only for the inpatient setting but for the outpatient setting as well. Vendors will be wise to address and support the delicate balance that surgeons must maintain between their inpatient hospital-based interests and their ambulatory interests relative to place of surgery and implant selection.
- Assess current levels of outpatient and ambulatory business relative to product sales; stand up resources to understand, plan and execute an ambulatory strategy.
- Evaluate whether inpatient products and services can be applied to the ambulatory setting or if new or modified products are required.
- Evaluate whether the sports medicine model of sales and service is an applicable model for joints and spine.
- Understand whether there is an opportunity to support and collaborate in the development of ambulatory protocols for joints and spine, patient oriented applications, pre-surgical patient education, site-specific instrument tray configurations, novel techniques and processes.
- When an ASC is physician-owned, there is potentially a substantial “first-mover advantage” for vendors that intentionally develop and execute an ambulatory strategy, because owners tend to be more price sensitive and less brand sensitive, but this too is likely to concretize over time.
Summary of Comments
COVID-19 will be an enduring guest in our healthcare environment; its impact likely vacillating between acute and chronic. Despite this, there is both need and opportunity for a dedicated ambulatory strategy for vendors. As vendors’ customers, whether physicians or hospitals, intentionally move cases to ambulatory settings, vendor services and strategies will need retooling. Essentially, vendors will need to more effectively “sync” with their ambulatory customers for product, service and strategy. It is a certainty that volumes will move, perhaps rapidly. For all stakeholders, a critical question looms, in the face of COVID: will they be proactive and realize the benefits, or reactive and become less competitive?

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
PV
Patrick Vega is Consulting Director for Vizient’s Excelerate and PPI Orthopedics. Mr. Vega consults to member hospitals, health systems and physicians in musculoskeletal services with a focus on high-value care by aligning cost, quality and performance.