Copy to clipboard
Copy to clipboard 
Preview
The purpose of this quarterly column is to introduce and discuss key considerations for device companies from the perspective of their customers: hospitals, health systems and physicians. This article provides a description of ambulatory settings and strategies, and suggests ways that device companies can capitalize on the shift from inpatient surgical settings to hospital outpatient departments, ambulatory surgery centers (ASCs) and outpatient sites of care. The collective contributors to this article hypothesize that device companies that better understand the outpatient setting can more effectively adapt their products, services and support to meet customer needs.
THE SITUATION
The historical model for orthopedic and spine procedures has been inpatient focused, resulting in high revenue and high margins and requiring extensive infrastructure and resources. The emerging model is both inpatient and outpatient. The principal reasons for this shift include:
- Patient preference for a least restrictive level of care coupled with the convenience of proximate and community-based care
- First-time or enhanced reimbursement for outpatient-based procedures, which might include reimbursement models like bundled payments or site-neutral reimbursement
- Improved technology and patient safety; these include pain management techniques, outpatient patient care pathways, minimally invasive surgical techniques, patient selection and highly defined treatment protocols
INPATIENT VS. OUTPATIENT GROWTH
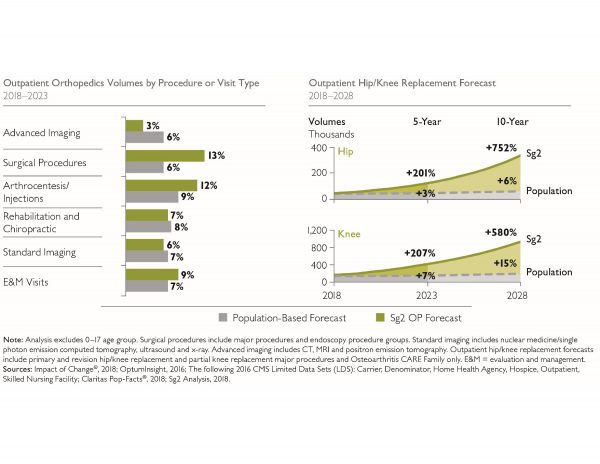
Orthopedic outpatient procedures are expected to surge in the coming years. The left-hand column in Exhibit 1 describes overall population increases in the U.S. and increased forecasts for orthopedic outpatient volume growth as captured in the population-based forecast bars. Due to the increased movement of higher acuity orthopedic procedures to outpatient settings, such as spine and joint replacement surgeries, Sg2 predicts a 13% increase in outpatient orthopedic surgeries in the next five years, outpacing the increase of population growth alone. In Exhibit 1 (right column), Sg2 projects that outpatient hip and knee replacement surgeries will increase over 200% in the next five years with growth projected to be 580% for hip replacement and 752% for knee replacement over the next ten years.
Exhibit 1: Orthopedic Outpatient Forecast
Source: Sg2 Report Orthopedics Service Line Snapshot 2018
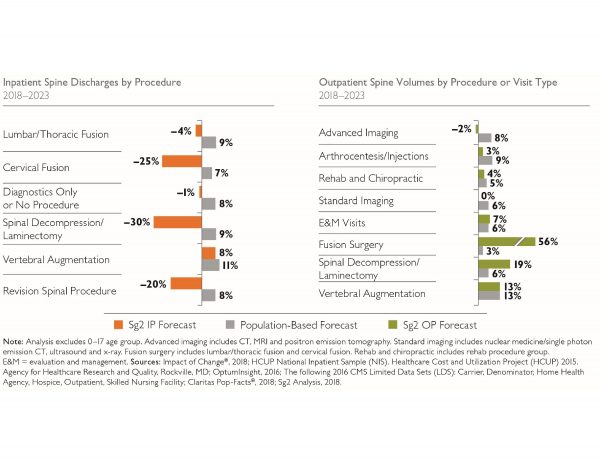
In Exhibit 2, population estimates show modest inpatient spine growth, while Sg2 projects mostly declines in inpatient procedures. Conversely, Sg2 projects growth of outpatient spine procedures; especially notable is Fusion Surgery at 56% growth between 2018 and 2023.
Exhibit 2: Spine Outpatient Forecast
Source: Sg2 Report Spine Service Line Snapshot 2018
WHERE DOES SURGERY OCCUR?
Exhibit 3 illustrates both places of care and considerations for selecting a place of care. The continuum of options includes hospital outpatient departments, which may be a dedicated same-day surgical suite or department or simply the use of the main operating room suites for same-day cases. ASCs are typically specialty focused on lines like orthopedics, spine, ENT and interventional pain management. It is worth noting that the four ownership models in ASC settings may dictate specific strategies for each.
Exhibit 3: Service Options and Considerations
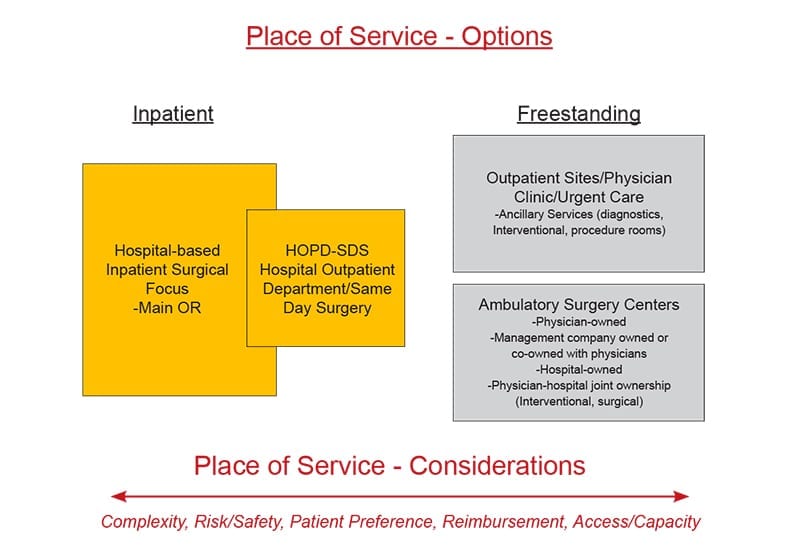
Source: Patrick Vega, Vizient
CMS IMPACT ON ASC TRENDS
Today, the Centers for Medicare & Medicaid Services (CMS) only reimburses for knee replacements performed in a hospital-based outpatient setting. Once CMS approves reimbursement for joint replacement at any site of care, 15% to 30% of clinically appropriate Medicare reimbursed patients are projected to exit the inpatient setting. Hospitals can expect that surgeons will elect to take clinically appropriate patients to ASCs, resulting in a net loss of inpatient. Further, the percentage of outpatient cases will not remain static; rather, the numbers will grow. Proactive vendors and health systems are devoting strategic and tactical resources to leverage the market reality rather than lag among competitors.
It is my observation that most hospitals and health systems are ill-prepared both strategically and tactically to capitalize on the outpatient opportunity. Often times hospitals anticipate that reimbursement will be lower on an outpatient basis, which certainly can be true. The challenge lies in that if they have not committed strategically and tactically to proactively move cases, they are at risk for ASCs (often physician owned) to more rapidly gear up and take market share. In simple terms, health systems risk losing a substantial number of these cases to more focused and better prepared physician competitors.
DEVICE COMPANY CONSIDERATIONS
Traditionally, the device company’s primary customer contact has been the surgeon, purchasing and supply chain. With the emergence of integrated delivery networks and the supply chain having more visibility as a strategic department, customers and decision-makers have increased in numbers and scope of influence. This shift requires skill sets beyond supporting the surgeon in the O.R. and negotiating for implant pricing; it requires expanded knowledge of hospital departments, cost containment strategies and clinical use of their products in patient care.
CUSTOMER PERSPECTIVE
We have solicited insight, opinion and expertise from a number of professionals with experience in outpatient care. Each brings a unique understanding of the opportunities and challenges of capturing and leveraging the burgeoning growth of outpatient care. Panelists’ perspectives may speak directly to vendor opportunity or may describe a system of care that proactive vendors can explore and innovate within.
Economic Incentives
Frank Cannata, President, The Cannata Group | Chestnut Hill, Massachusetts
Mr. Cannata leads a consulting group supporting vendors, following years as an owner and Agent Principal for Biosystems Spine, a Stryker Spine affiliate. Mr. Cannata also validates the shift of historically inpatient bound spine procedures moving to outpatient settings. Those types of cases can include anterior cervical discectomy and fusion, micro discectomy, cervical discectomy, foraminotomy and uncomplicated lumbar fusion, depending on the skill and experience of the surgeon.
Further, state by state, Certificate of Need regulations often times curb the growth of outpatient surgery centers, particularly those owned exclusively by physicians. Mr. Cannata cites a recent example of joint surgeons taking cases out of the inpatient setting to physician owned ASCs located across state borders. In addition to removing cases out of their primary hospitals, the surgeons have negotiated more favorable pricing than their hospitals, potentially creating additional tension among the hospital, surgeon and device company.
Clark Charlton, Chief Strategy Officer, Relatable Healthcare | Nashville, Tennessee
Mr. Charlton leads strategy for Relatable Healthcare, a business intelligence firm focused on the outpatient care space, supporting management and clinical teams with extensive data-driven insights. Their business intelligence platform objectively compares medical devices, analyzes usage and offers intelligent recommendations on ways to optimize clinical and economic decisions to best treat patients. Medical device companies and ASCs need to consider the following to align on price points/reimbursements, in many cases lower than inpatient settings for implants:
- Pursue regional or national pricing contracts to increase purchase volume (ASC management companies)
- Drive high compliance contracts through supplier standardization (ASC management companies)
- Reduce sales representative service models that require O.R. staff to be self-sufficient to support procedures
Chris Stine, JD, MBA, Director, Bundled Payments & Corporate Compliance Officer, Regent Surgical Health | Westchester, Illinois
Regent Surgical offers a full suite of consulting services in the outpatient surgery setting: strategy assessment, development, management, turnaround, revenue cycle management, bundled payment and joint ventures. Regent’s Director of Bundled Payments Chris Stine says, “Employers are driving payment reform, looking for alternatives, designing benefit programs and leveraging their resources to bridge the information gap. And, once they take the proactive step of looking for ways to improve their healthcare costs, it becomes apparent that the more expensive hospitals in the cost continuum for surgical care can be complemented with an outpatient facility that can often lead to higher patient satisfaction and high-quality outcomes.”
According to Mr. Stine, for the joint and spine surgeon there is a substantial economic incentive to move cases to an ASC, especially when they have an ownership. For the hospital, movement of cases to the outpatient setting may alleviate capacity constraints and make room for higher acuity cases. Key influences and underlying rationale driving outpatient growth include physician alignment and the rise of site neutral payment (especially for hospitals and physicians), increased awareness of costs for orthopedics and spine cases, particularly the cost of implants. Further, payors are incentivizing providers to care about these costs. These drivers are often manifested with a focus on standardization of implants through the use of formulary and bench pricing. Moreover, surgeons may see additional economic benefit through shared savings models.
Stine poses another question relative to outpatient care, which is, “How can we think more creatively? Our experience suggests that success is not about evolving the old without leaving a comfort zone, because that zone slowly evaporates. Success is about knowing when the time is right to break the mold, revolutionize or even cannibalize an existing operating model for a proven emerging model.”
Jessica Cooper, MS, Chief Administrative Officer, Neurosciences Service Line, University of Pennsylvania Health System | Philadelphia, Pennsylvania
Penn Medicine is a not-for-profit academic medical system of six hospitals with about 3,000 licensed beds and hundreds of outpatient locations throughout the region. Penn draws patients from Pennsylvania, Delaware, New Jersey and beyond. Penn performs approximately 2,250 spine surgical cases (IP + OP) and about 3,300 injections annually at its three Philadelphia-based hospitals. Strategy development and implementation are driven by multiple forces: market dynamics, reimbursement, value based care, quality improvement, performance improvement and physician recruitment.
Outpatient locations for spine care include multi-specialty spine centers and community-based practices in which spine specialists are co-located with primary care. Penn Medicine is strategically focused on outpatient services and presently derives about 60% of its overall revenue from them. The model has a greater emphasis on same-day surgery in the main O.R. and less emphasis on outpatient surgery centers. Across the system, as well as at Penn’s new brick and mortar comprehensive Spine Center at Pennsylvania Hospital, spine care incorporates the following specialties: neurosurgery, orthopedics, neurophysiology, anesthesia/pain medicine, physical medicine and rehabilitation (PM&R) and physical therapy.
Patient access and navigation is the prevailing model utilizing patient care pathways as a differentiator in this highly competitive market. Pathways include physiatry, anesthesia and pain, and both orthopedic surgery and neurological surgery, all supported by clinical nurse navigation.
Ms. Cooper is explicit in defining the challenge of delivering high quality spine care. “Developing an integrated outpatient strategy for a single hospital requires diligence, across six hospitals and multiple departments…that’s the challenge.” Additionally, she observes, with integration and work to minimize variation being the goals, it requires sustained focus, as silo retrenchment naturally occurs.
Surgeons highly prize their sales representatives for their knowledge, and these relationships can support product preference. Historically, when evaluating vendor costs, the prevailing strategy has been consolidation of vendors driven by engagement of surgeons, detailed analysis, renegotiation for better pricing, identification and appointment of interchangeable products, reviews of costs and reductions in variation of use. There is an overall philosophy relative to vendors; integrating and coordinating use of products with cost and organizational goals. Ms. Cooper used the term “leaning in” to describe the purposeful and deliberate strategy to engage as a system with vendors.
Patient Incentives
Joe Tomaro Ph.D., Consulting Director, Advisory Solutions, Vizient Inc. | Centennial, Colorado
Vizient’s Advisory Solutions group supports its membership in delivering high-value care by aligning cost, quality and performance. With Dr. Tomaro’s accomplished background as a physical therapist, healthcare consultant and advisor on outpatient care, he brings a broad perspective on the intersection of provider, vendor and hospital. He shared the following insights on vendor products that support joint replacement in the outpatient setting.
There has been a significant increase in healthcare apps with some focused on helping to guide patients through pre- and post-operative care elements for elective and complex surgical procedures, many developed by orthopedic device companies. Examples of supportive apps include:
- Non-OEM: HealthLoop, Force Therapeutics, Pulse, Wellbe
- OEM-related: Zimmer Biomet’s mymobility, Stryker’s JointCOACH, DePuy Synthes’ CareSense
Most have features that include patient education, forums for patient/provider communication, collection of patient reported outcomes measures (PROMS) and rehabilitation programs. While relatively new, peer-reviewed research studies have demonstrated improved patient education, increased satisfaction, better outcomes and decreased cost.
Patient-facing apps may have specific benefits for outpatient joint replacement surgeries: helping ease patient’s anxiety in advance of complex outpatient surgery, collection of outcomes information reporting to surgeon, payor and provider organizations to substantiate quality claims, benchmark against best performers and improve care. Additionally, outcomes collection and reporting can be integral to bundled payments for outpatient procedures.
One key concern for same-day patients is a lack of connection with their surgeon, particularly if there are issues during the immediate post-operative period. Apps can effectively bridge this gap with well-crafted pre-operative messages and immediately post-operatively to specifically educate patients on routine activities to be performed, and coaching on what is and is not normal during recovery. This increased level of education along with the ability to easily exchange texts or even images with their provider through a secure platform can help to assuage a patient’s anxiety level, improve their satisfaction and in the event of an adverse outcome, informing them of required action.
Since outpatient joint replacement is a relatively new procedure, many payors want outcomes information as part of their agreements with providers. Many of the apps on the market have shown to have as high as a 75% collection of PROMS data at one year post-operatively with limited patient follow-up needed for completion. For providers and payers, outcomes data can be essential to validate that comparable or better clinical outcomes are achievable in outpatient settings.
Product Incentives
James Shea, Administrator, Black Hills Neurosurgery & Spine and President of NERVES (Neurosurgery Executives’ Resource Value and Education Society) | Rapid City, South Dakota
Mr. Shea believes that it is reasonable to anticipate that in the outpatient setting, the traditional value analysis committee and processes will be equally applicable if not even more muscular because of physician ownership of the practice’s related specialty surgical site; Black Hills Surgical Hospital.
Relative to vendors, the goal of the Black Hills value analysis process is to deliver and ensure a streamlined and effective process for reviewing new products while seeking input from all constituencies. Vendor overtures and surgeons are often the initial source of new product introductions. For the hospital, the value analysis process occurs through an operations committee comprising administration and physicians. Product sponsors must present to the operations committee in a prescribed process. Purchasing staff conduct research on the product in terms of benefit: clinical, cost and economics.
Tim Skinner, Director of Purchasing and Project Development, Black Hills Surgical Hospital | Rapid City, South Dakota
Mr. Skinner manages the product evaluation process and observed that, to date, there have been no outpatient-specific product introductions. Rather, instruments and implants, if used for outpatient cases, are the same products used for similar cases in the hospital inpatient setting. While the hospital’s favorable product pricing reflects an underlying strategy of single-source vendor contracts for joints and spine, there is openness to new products and services conforming to their clinical and value analysis process.
VENDOR TAKEAWAYS
There are a number of takeaways in the outpatient setting that include continuing price pressure driven by specialty hospitals with outpatient services, often with physician ownership. Outpatient providers will pursue preferential implant pricing to drive improved margins as well as to competitively price their services for such reimbursement models as bundled payment. One interesting consequence of this could be where the vendor offers different pricing to the same physician depending on their site of service, be at inpatient or outpatient. Areas of further consideration include:
- Presumably, vendors are interested in maintaining their surgeons’ products not only for the inpatient setting but for outpatient as well; additionally, vendors will be wise to address and support the delicate balance that surgeons must maintain between their inpatient hospital-based interests and their outpatient interests relative to place of surgery and implant selection
- Assess current levels of outpatient and outpatient business relative to product sales, stand up resources to understand, plan and execute an outpatient strategy
- Evaluate whether inpatient products and services can be applied to the outpatient setting, or are new or modified products required for the setting
- Evaluate whether the sports medicine model of sales and service is most applicable and a corollary for joints and spine
- Understand whether there is an opportunity to support and collaborate in the development of outpatient protocols for joints and spine; patient oriented applications, pre-surgical patient education, site–specific instrument tray configurations, novel techniques and processes
- Margin per unit for implants is likely to decrease
- For the vendor, how can I tie in my implant into other complementary products and ancillary products or services?
- The outpatient migration of cases will continue to grow in volume, variety and complexity as technology, protocols and pain management evolve
- Is there potentially a “first mover advantage” for vendors that intentionally develop and execute an outpatient strategy?
Summary
There is both need and opportunity for a dedicated outpatient strategy for device companies. As their customers, whether physicians or hospitals, intentionally move cases to an outpatient setting, device company services and strategies will need retooling. Essentially, can you more effectively “sync” with your outpatient customers from product, service and strategy perspectives. It is a certainty that volumes will move, perhaps rapidly. For all stakeholders, a critical question looms: will they be proactive and realize the benefits, or reactive and become less competitive?
Preview
The purpose of this quarterly column is to introduce and discuss key considerations for device companies from the perspective of their customers: hospitals, health systems and physicians. This article provides a description of ambulatory settings and strategies, and suggests ways that device companies can capitalize on the shift from...
Preview
The purpose of this quarterly column is to introduce and discuss key considerations for device companies from the perspective of their customers: hospitals, health systems and physicians. This article provides a description of ambulatory settings and strategies, and suggests ways that device companies can capitalize on the shift from inpatient surgical settings to hospital outpatient departments, ambulatory surgery centers (ASCs) and outpatient sites of care. The collective contributors to this article hypothesize that device companies that better understand the outpatient setting can more effectively adapt their products, services and support to meet customer needs.
THE SITUATION
The historical model for orthopedic and spine procedures has been inpatient focused, resulting in high revenue and high margins and requiring extensive infrastructure and resources. The emerging model is both inpatient and outpatient. The principal reasons for this shift include:
- Patient preference for a least restrictive level of care coupled with the convenience of proximate and community-based care
- First-time or enhanced reimbursement for outpatient-based procedures, which might include reimbursement models like bundled payments or site-neutral reimbursement
- Improved technology and patient safety; these include pain management techniques, outpatient patient care pathways, minimally invasive surgical techniques, patient selection and highly defined treatment protocols
INPATIENT VS. OUTPATIENT GROWTH
Orthopedic outpatient procedures are expected to surge in the coming years. The left-hand column in Exhibit 1 describes overall population increases in the U.S. and increased forecasts for orthopedic outpatient volume growth as captured in the population-based forecast bars. Due to the increased movement of higher acuity orthopedic procedures to outpatient settings, such as spine and joint replacement surgeries, Sg2 predicts a 13% increase in outpatient orthopedic surgeries in the next five years, outpacing the increase of population growth alone. In Exhibit 1 (right column), Sg2 projects that outpatient hip and knee replacement surgeries will increase over 200% in the next five years with growth projected to be 580% for hip replacement and 752% for knee replacement over the next ten years.
Exhibit 1: Orthopedic Outpatient Forecast
Source: Sg2 Report Orthopedics Service Line Snapshot 2018
In Exhibit 2, population estimates show modest inpatient spine growth, while Sg2 projects mostly declines in inpatient procedures. Conversely, Sg2 projects growth of outpatient spine procedures; especially notable is Fusion Surgery at 56% growth between 2018 and 2023.
Exhibit 2: Spine Outpatient Forecast
Source: Sg2 Report Spine Service Line Snapshot 2018
WHERE DOES SURGERY OCCUR?
Exhibit 3 illustrates both places of care and considerations for selecting a place of care. The continuum of options includes hospital outpatient departments, which may be a dedicated same-day surgical suite or department or simply the use of the main operating room suites for same-day cases. ASCs are typically specialty focused on lines like orthopedics, spine, ENT and interventional pain management. It is worth noting that the four ownership models in ASC settings may dictate specific strategies for each.
Exhibit 3: Service Options and Considerations
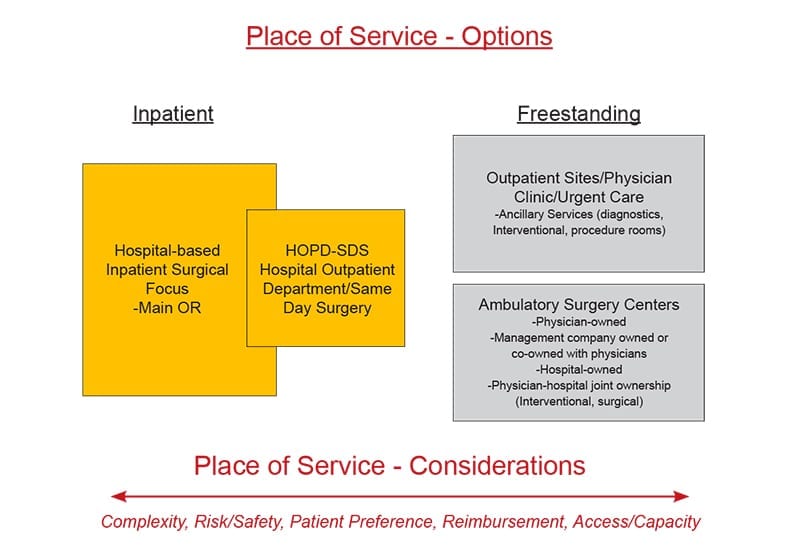
Source: Patrick Vega, Vizient
CMS IMPACT ON ASC TRENDS
Today, the Centers for Medicare & Medicaid Services (CMS) only reimburses for knee replacements performed in a hospital-based outpatient setting. Once CMS approves reimbursement for joint replacement at any site of care, 15% to 30% of clinically appropriate Medicare reimbursed patients are projected to exit the inpatient setting. Hospitals can expect that surgeons will elect to take clinically appropriate patients to ASCs, resulting in a net loss of inpatient. Further, the percentage of outpatient cases will not remain static; rather, the numbers will grow. Proactive vendors and health systems are devoting strategic and tactical resources to leverage the market reality rather than lag among competitors.
It is my observation that most hospitals and health systems are ill-prepared both strategically and tactically to capitalize on the outpatient opportunity. Often times hospitals anticipate that reimbursement will be lower on an outpatient basis, which certainly can be true. The challenge lies in that if they have not committed strategically and tactically to proactively move cases, they are at risk for ASCs (often physician owned) to more rapidly gear up and take market share. In simple terms, health systems risk losing a substantial number of these cases to more focused and better prepared physician competitors.
DEVICE COMPANY CONSIDERATIONS
Traditionally, the device company’s primary customer contact has been the surgeon, purchasing and supply chain. With the emergence of integrated delivery networks and the supply chain having more visibility as a strategic department, customers and decision-makers have increased in numbers and scope of influence. This shift requires skill sets beyond supporting the surgeon in the O.R. and negotiating for implant pricing; it requires expanded knowledge of hospital departments, cost containment strategies and clinical use of their products in patient care.
CUSTOMER PERSPECTIVE
We have solicited insight, opinion and expertise from a number of professionals with experience in outpatient care. Each brings a unique understanding of the opportunities and challenges of capturing and leveraging the burgeoning growth of outpatient care. Panelists’ perspectives may speak directly to vendor opportunity or may describe a system of care that proactive vendors can explore and innovate within.
Economic Incentives
Frank Cannata, President, The Cannata Group | Chestnut Hill, Massachusetts
Mr. Cannata leads a consulting group supporting vendors, following years as an owner and Agent Principal for Biosystems Spine, a Stryker Spine affiliate. Mr. Cannata also validates the shift of historically inpatient bound spine procedures moving to outpatient settings. Those types of cases can include anterior cervical discectomy and fusion, micro discectomy, cervical discectomy, foraminotomy and uncomplicated lumbar fusion, depending on the skill and experience of the surgeon.
Further, state by state, Certificate of Need regulations often times curb the growth of outpatient surgery centers, particularly those owned exclusively by physicians. Mr. Cannata cites a recent example of joint surgeons taking cases out of the inpatient setting to physician owned ASCs located across state borders. In addition to removing cases out of their primary hospitals, the surgeons have negotiated more favorable pricing than their hospitals, potentially creating additional tension among the hospital, surgeon and device company.
Clark Charlton, Chief Strategy Officer, Relatable Healthcare | Nashville, Tennessee
Mr. Charlton leads strategy for Relatable Healthcare, a business intelligence firm focused on the outpatient care space, supporting management and clinical teams with extensive data-driven insights. Their business intelligence platform objectively compares medical devices, analyzes usage and offers intelligent recommendations on ways to optimize clinical and economic decisions to best treat patients. Medical device companies and ASCs need to consider the following to align on price points/reimbursements, in many cases lower than inpatient settings for implants:
- Pursue regional or national pricing contracts to increase purchase volume (ASC management companies)
- Drive high compliance contracts through supplier standardization (ASC management companies)
- Reduce sales representative service models that require O.R. staff to be self-sufficient to support procedures
Chris Stine, JD, MBA, Director, Bundled Payments & Corporate Compliance Officer, Regent Surgical Health | Westchester, Illinois
Regent Surgical offers a full suite of consulting services in the outpatient surgery setting: strategy assessment, development, management, turnaround, revenue cycle management, bundled payment and joint ventures. Regent’s Director of Bundled Payments Chris Stine says, “Employers are driving payment reform, looking for alternatives, designing benefit programs and leveraging their resources to bridge the information gap. And, once they take the proactive step of looking for ways to improve their healthcare costs, it becomes apparent that the more expensive hospitals in the cost continuum for surgical care can be complemented with an outpatient facility that can often lead to higher patient satisfaction and high-quality outcomes.”
According to Mr. Stine, for the joint and spine surgeon there is a substantial economic incentive to move cases to an ASC, especially when they have an ownership. For the hospital, movement of cases to the outpatient setting may alleviate capacity constraints and make room for higher acuity cases. Key influences and underlying rationale driving outpatient growth include physician alignment and the rise of site neutral payment (especially for hospitals and physicians), increased awareness of costs for orthopedics and spine cases, particularly the cost of implants. Further, payors are incentivizing providers to care about these costs. These drivers are often manifested with a focus on standardization of implants through the use of formulary and bench pricing. Moreover, surgeons may see additional economic benefit through shared savings models.
Stine poses another question relative to outpatient care, which is, “How can we think more creatively? Our experience suggests that success is not about evolving the old without leaving a comfort zone, because that zone slowly evaporates. Success is about knowing when the time is right to break the mold, revolutionize or even cannibalize an existing operating model for a proven emerging model.”
Jessica Cooper, MS, Chief Administrative Officer, Neurosciences Service Line, University of Pennsylvania Health System | Philadelphia, Pennsylvania
Penn Medicine is a not-for-profit academic medical system of six hospitals with about 3,000 licensed beds and hundreds of outpatient locations throughout the region. Penn draws patients from Pennsylvania, Delaware, New Jersey and beyond. Penn performs approximately 2,250 spine surgical cases (IP + OP) and about 3,300 injections annually at its three Philadelphia-based hospitals. Strategy development and implementation are driven by multiple forces: market dynamics, reimbursement, value based care, quality improvement, performance improvement and physician recruitment.
Outpatient locations for spine care include multi-specialty spine centers and community-based practices in which spine specialists are co-located with primary care. Penn Medicine is strategically focused on outpatient services and presently derives about 60% of its overall revenue from them. The model has a greater emphasis on same-day surgery in the main O.R. and less emphasis on outpatient surgery centers. Across the system, as well as at Penn’s new brick and mortar comprehensive Spine Center at Pennsylvania Hospital, spine care incorporates the following specialties: neurosurgery, orthopedics, neurophysiology, anesthesia/pain medicine, physical medicine and rehabilitation (PM&R) and physical therapy.
Patient access and navigation is the prevailing model utilizing patient care pathways as a differentiator in this highly competitive market. Pathways include physiatry, anesthesia and pain, and both orthopedic surgery and neurological surgery, all supported by clinical nurse navigation.
Ms. Cooper is explicit in defining the challenge of delivering high quality spine care. “Developing an integrated outpatient strategy for a single hospital requires diligence, across six hospitals and multiple departments…that’s the challenge.” Additionally, she observes, with integration and work to minimize variation being the goals, it requires sustained focus, as silo retrenchment naturally occurs.
Surgeons highly prize their sales representatives for their knowledge, and these relationships can support product preference. Historically, when evaluating vendor costs, the prevailing strategy has been consolidation of vendors driven by engagement of surgeons, detailed analysis, renegotiation for better pricing, identification and appointment of interchangeable products, reviews of costs and reductions in variation of use. There is an overall philosophy relative to vendors; integrating and coordinating use of products with cost and organizational goals. Ms. Cooper used the term “leaning in” to describe the purposeful and deliberate strategy to engage as a system with vendors.
Patient Incentives
Joe Tomaro Ph.D., Consulting Director, Advisory Solutions, Vizient Inc. | Centennial, Colorado
Vizient’s Advisory Solutions group supports its membership in delivering high-value care by aligning cost, quality and performance. With Dr. Tomaro’s accomplished background as a physical therapist, healthcare consultant and advisor on outpatient care, he brings a broad perspective on the intersection of provider, vendor and hospital. He shared the following insights on vendor products that support joint replacement in the outpatient setting.
There has been a significant increase in healthcare apps with some focused on helping to guide patients through pre- and post-operative care elements for elective and complex surgical procedures, many developed by orthopedic device companies. Examples of supportive apps include:
- Non-OEM: HealthLoop, Force Therapeutics, Pulse, Wellbe
- OEM-related: Zimmer Biomet’s mymobility, Stryker’s JointCOACH, DePuy Synthes’ CareSense
Most have features that include patient education, forums for patient/provider communication, collection of patient reported outcomes measures (PROMS) and rehabilitation programs. While relatively new, peer-reviewed research studies have demonstrated improved patient education, increased satisfaction, better outcomes and decreased cost.
Patient-facing apps may have specific benefits for outpatient joint replacement surgeries: helping ease patient’s anxiety in advance of complex outpatient surgery, collection of outcomes information reporting to surgeon, payor and provider organizations to substantiate quality claims, benchmark against best performers and improve care. Additionally, outcomes collection and reporting can be integral to bundled payments for outpatient procedures.
One key concern for same-day patients is a lack of connection with their surgeon, particularly if there are issues during the immediate post-operative period. Apps can effectively bridge this gap with well-crafted pre-operative messages and immediately post-operatively to specifically educate patients on routine activities to be performed, and coaching on what is and is not normal during recovery. This increased level of education along with the ability to easily exchange texts or even images with their provider through a secure platform can help to assuage a patient’s anxiety level, improve their satisfaction and in the event of an adverse outcome, informing them of required action.
Since outpatient joint replacement is a relatively new procedure, many payors want outcomes information as part of their agreements with providers. Many of the apps on the market have shown to have as high as a 75% collection of PROMS data at one year post-operatively with limited patient follow-up needed for completion. For providers and payers, outcomes data can be essential to validate that comparable or better clinical outcomes are achievable in outpatient settings.
Product Incentives
James Shea, Administrator, Black Hills Neurosurgery & Spine and President of NERVES (Neurosurgery Executives’ Resource Value and Education Society) | Rapid City, South Dakota
Mr. Shea believes that it is reasonable to anticipate that in the outpatient setting, the traditional value analysis committee and processes will be equally applicable if not even more muscular because of physician ownership of the practice’s related specialty surgical site; Black Hills Surgical Hospital.
Relative to vendors, the goal of the Black Hills value analysis process is to deliver and ensure a streamlined and effective process for reviewing new products while seeking input from all constituencies. Vendor overtures and surgeons are often the initial source of new product introductions. For the hospital, the value analysis process occurs through an operations committee comprising administration and physicians. Product sponsors must present to the operations committee in a prescribed process. Purchasing staff conduct research on the product in terms of benefit: clinical, cost and economics.
Tim Skinner, Director of Purchasing and Project Development, Black Hills Surgical Hospital | Rapid City, South Dakota
Mr. Skinner manages the product evaluation process and observed that, to date, there have been no outpatient-specific product introductions. Rather, instruments and implants, if used for outpatient cases, are the same products used for similar cases in the hospital inpatient setting. While the hospital’s favorable product pricing reflects an underlying strategy of single-source vendor contracts for joints and spine, there is openness to new products and services conforming to their clinical and value analysis process.
VENDOR TAKEAWAYS
There are a number of takeaways in the outpatient setting that include continuing price pressure driven by specialty hospitals with outpatient services, often with physician ownership. Outpatient providers will pursue preferential implant pricing to drive improved margins as well as to competitively price their services for such reimbursement models as bundled payment. One interesting consequence of this could be where the vendor offers different pricing to the same physician depending on their site of service, be at inpatient or outpatient. Areas of further consideration include:
- Presumably, vendors are interested in maintaining their surgeons’ products not only for the inpatient setting but for outpatient as well; additionally, vendors will be wise to address and support the delicate balance that surgeons must maintain between their inpatient hospital-based interests and their outpatient interests relative to place of surgery and implant selection
- Assess current levels of outpatient and outpatient business relative to product sales, stand up resources to understand, plan and execute an outpatient strategy
- Evaluate whether inpatient products and services can be applied to the outpatient setting, or are new or modified products required for the setting
- Evaluate whether the sports medicine model of sales and service is most applicable and a corollary for joints and spine
- Understand whether there is an opportunity to support and collaborate in the development of outpatient protocols for joints and spine; patient oriented applications, pre-surgical patient education, site–specific instrument tray configurations, novel techniques and processes
- Margin per unit for implants is likely to decrease
- For the vendor, how can I tie in my implant into other complementary products and ancillary products or services?
- The outpatient migration of cases will continue to grow in volume, variety and complexity as technology, protocols and pain management evolve
- Is there potentially a “first mover advantage” for vendors that intentionally develop and execute an outpatient strategy?
Summary
There is both need and opportunity for a dedicated outpatient strategy for device companies. As their customers, whether physicians or hospitals, intentionally move cases to an outpatient setting, device company services and strategies will need retooling. Essentially, can you more effectively “sync” with your outpatient customers from product, service and strategy perspectives. It is a certainty that volumes will move, perhaps rapidly. For all stakeholders, a critical question looms: will they be proactive and realize the benefits, or reactive and become less competitive?

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
PV
Patrick Vega is Consulting Director for Vizient’s Excelerate and PPI Orthopedics. Mr. Vega consults to member hospitals, health systems and physicians in musculoskeletal services with a focus on high-value care by aligning cost, quality and performance.