Copy to clipboard
Copy to clipboard 
Dear Members and Subscribers,
We are compelled to re-share this succinct summary of the 234,812-word Patient Protection and Affordable Care Act (PPACA). While several elements have been and continue to be modified, the overall constitutionality of its contents are under review by the U.S. Supreme Court. Many are chiming in to offer their predictions on its fate. We possess no crystal ball through which to forecast our future, but we can provide this digestible version of the Act along with continued, concise reporting of its impact.
Summary of the Patient Protection and Affordable Care Act: QUALITY, AFFORDABLE HEALTH CARE FOR ALL AMERICANS
Immediate Improvements in Health Care Coverage for All Americans
Expand Coverage/Improve Access
Mandate that employers with more than 200 employees automatically enroll employees in health insurance plans offered by the employer (employees may opt out). (2014) Companies with 50 or fewer employees are exempt from fees.
Those with fewer than 200 employees do not have to offer coverage; however, those with more than 50 employees must pay a fee ($2,000 for each full-time employee excluding the first 30) if even one of their full-time employees is receiving a government subsidy for private insurance. Employers with more than 50 employees that offer coverage and have employees receiving subsidies can pay the lower of $3,000 per employee receiving a subsidy or $2,000 per full-time employee.
Provide tax credits to smaller employers (25 or fewer employees and average annual wages of less than $50,000) for purchasing employee health insurance (2010-2013). The employer must contribute at least 50% of total premium cost or an amount to be established by the government. The size of the credit will vary based on company size, i.e., companies with 10 or fewer employees and average annual wages of less than $25,000 get a credit equal to 35% of the employer’s contribution to insurance costs. In 2014 and beyond, the tax credit increases to a maximum of 50% of the employer’s contribution.
Limit the deductible in insurance plans for small groups to no more than $2,000 for individuals and $4,000 for families unless offset by contributions offered by the insurance plan. (2014)
Prohibit cancellation of private insurance coverage except in cases of fraud. (September 2010)
Prohibit denial of coverage based on a pre-existing condition.
Prohibit insurers from refusing coverage for patients who have “consumed” a dollar value of services greater than a pre-determined lifetime limit. (2014)
Expand Medicaid to all individuals under 65 with incomes at or below 133% of the Federal Poverty Level ($10,830 for individuals and $22,050 for a family of four). (Prior to this legislation, not all low-income individuals could avail themselves of Medicaid and eligibility varied from state to state.)
Provide premium credits and cost-sharing subsidies to individuals and families who fall below 400% of the Federal Poverty Level, with some restrictions. (2014)
Establish state-based health exchanges to allow individuals and businesses with fewer than 100 employees to pool together to purchase insurance (2014), with larger businesses (100+ employees) able to participate in 2017. The Federal Government will also offer subsidies to low-income individuals to purchase insurance through the exchanges.
Offer (Federal government through private insurers) at least two multi-state health insurance plans in each state health insurance exchange, with at least one being a non-profit entity. (2014)
Allow parents to keep their children on their health insurance plans up to age 26. (September 2010)
Reduce Costs/Reform Government Programs
Reduce Medicare payments to hospitals by adjusting reimbursement increases to below the market basket beginning with a 1/4 percentage point reduction in 2010 and 2011. (0.1% in 2012 and 2013, 0.2% in 2015 and 2016, and 0.75% in 2017-2019)
Reduce payments to inpatient, outpatient and ASC facilities beginning in 2012.
Apply a productivity reduction to future Medicare payment updates.
Reduce by 75% Medicare and Medicaid payments to “disproportionate share hospitals” (hospitals that care for more costly indigent patients). (2014)
Create the Independent Payment Advisory Board to hold growth in Medicare spending per beneficiary to a certain level. Recommendations from the Board are due by 1/15/2014, with implementation in 2015 unless Congress comes up with its own mechanism for bringing costs in line. Limit growth to GDP growth per capita plus one percentage point beginning in 2018.
Adjust Medicare Advantage payments downward. (2011) (Approximately 25% of Medicare beneficiaries now avail themselves of the Advantage program, paying more to receive additional benefits beyond those provided with basic Medicare coverage.)
Prohibit new physician-owned hospitals, with expansion of existing hospitals requiring approval from the Secretary of HHS. (December 31, 2010)
Require the Secretary of HHS to evaluate and adjust “misvalued” Relative Value Units with a view to corralling those that are the fastest growing in utilization; reflect new technologies or services; have low relative values… (Immediately)
Encourage hospitals and doctors to organize as accountable care organizations (ACOs) to provide coordinated care, encourage investment in infrastructure and increase quality and efficiency by redesigning healthcare delivery processes. (2012) If the ACO saves money, Medicare will share the savings with the ACO, with the ACO distributing savings to its participating hospitals and physicians.
Investigate using a single payment for all services involved in an episode of care for certain treatments (to be chosen by the Secretary of HHS) with the goal to reduce the cost of treatment while not reducing quality. (Medicaid 2012, Medicare 2013)
Extend gainsharing demonstration projects through 2011.
Improve Quality
Expand comparative effectiveness research program (now the Patient-Centered Outcomes Research Institute) and its funding. Note that the legislation indicates that the Institute may not create treatment mandates or practice guidelines nor can it make recommendations for payment coverage. Also, the legislation specifically mentions using comparative effectiveness research to compare medical devices. (Immediately)
Establish the Medicare Innovation Center with $1 billion/year in funding, to test different payment systems to reduce cost and improve quality. (2011)
Mandate physician participation in the Physician Quality Reporting Initiative and penalize physicians who do not satisfactorily report by imposing a 1.5% cut in pay in 2015 and 2% in 2016 and thereafter.
Add a value-based modifier to physicians’ Medicare fee schedule calculation based on quality and cost of treatment to redistribute money to the most cost-efficient physicians. (2017)
Mandate that private insurers (on all health plans) spend a specified proportion of premium dollars (80% or 85% depending on the market being serviced) on clinical services and quality enhancements or measures. (2011)
Add a 1% payment penalty to those hospitals that rank in the top 25% for hospital-acquired conditions; to be applied each year. (2015)
Reduce DRG payments to hospitals deemed to have “excess” readmissions (as determined by HHS), with a 1% reduction in 2013, moving to 3% by 2015.
Redistribute money to the most cost-efficient hospitals based on high quality scores or improvement in scores (calculated based on certain quality measures and cost per beneficiary for certain procedures as determined by HHS). Medicare will pay for the incentives by decreasing base DRG amounts for the procedures, beginning with a 1% reduction in 2013 and ramping to a total 2% reduction in 2017. (Similar programs may be developed for ASCs, SNFs and home health agencies. HHS must report to Congress on these initiatives by 1/1/11.)
Increase Focus on Wellness/Prevention
Mandate that private health plans provide coverage, with no out-of-pocket expense, of “proven” preventive services and immunizations, preventive care for children and adolescents and certain additional preventive care and screenings for women. (2010) A similar mandate takes effect for Medicare and Medicaid in 2011.
Promote wellness programs through incentives to employers, e.g. grants to small employers who establish wellness programs (2011) and ability of larger employers to offer their employees rewards like premium discounts if they participate in wellness programs and meet certain requirements. (2014)
Promote growth in the supply of primary care physicians by paying a 10% bonus to primary care physicians for five years. (2011-2015) (May also be seen as a way to reduce costs, since patients may not require specialist care.)
Promote growth in the supply of general surgeons with a 10% bonus to general surgeons for major surgical procedures in geographies deemed to have a shortage of general surgeons. (2011-2015) (May also be seen as a way to reduce costs, since patients may not require specialist care.)
Redistribute unused residency positions to primary care and general surgery and use
scholarships and loans to support training of primary care physicians. (2010)
Funding the Program
Mandate that all individuals purchase health insurance and impose a fine of $695 per individual ($2,085 maximum per family) for those who do not. Fines may not exceed 2.5% of taxable income. (2014)
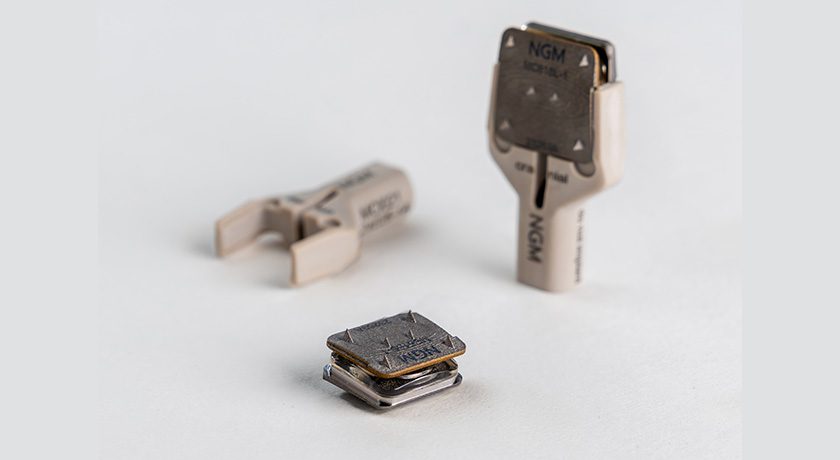
Impose a tax deductible medical device fee of 2.3% of U.S. sales of non-retail medical devices to be paid by manufacturers. (Calendar year 2013 revenues)
Impose a 40% fee on insurance companies for “Cadillac” plans, those that offer an aggregate value of more than $10,200 for individuals or $27,500 for family coverage, with the 40% applied to every dollar in value over these amounts. (2018)
Impose fees of $47.5 billion on private insurance companies from 2014 to 2018, as well as an aggregate of $25 billion from 2014 to 2016 to fund a temporary reinsurance program to cover high-risk individuals with pre-existing conditions. After 2018, companies must pay what they paid in the previous year increased by the rate of premium growth.
Impose $16.7 billion in fees on pharmaceutical companies from 2013 to 2019, and $2.8 billion per year thereafter.
Require that pharmaceutical companies provide deeper discounts and rebates for drugs sold to Medicare and Medicaid.
Increase to 2.35% (from 1.45%) the Medicare withholding tax on individuals who make more than $200,000, and joint filers making more than $250,000. (2013)
Impose a 3.8% tax for capital gains and other unearned income on individuals earning more than $200,000 and joint filers making more than $250,000. (2013)
Limit to $500,000 the amount of an individual’s pay that health care insurance companies may deduct as a business expense. (2010)
Transparency – Physician Payment Sunshine Provisions
The “Sunshine” provisions mandate that manufacturers disclose electronically the following information to the government:
All transfers of value to health care providers including individual payments of $10 or more or aggregate payments of $100 or more. (2012) After 2012, amounts will increase by the CPI. Manufacturers need not disclose product samples for patient use, educational materials for patient use, loans of evaluation devices, discounts and rebates, in-kind charity items, profit distributions from publicly-traded securities, health benefits to providers who are employees and payment for non-medical services to licensed non-medical professionals. Furthermore, disclosure of clinical research and product development agreements may be delayed until the product has been cleared for marketing or four years after the date of payment to the healthcare provider, whichever is earlier.
Ownership or investment interest (other than an ownership or investment interest in a publicly traded security and mutual fund) held by a physician (or an immediate family member of such physician) in the applicable manufacturer or applicable group purchasing organization during the preceding year.
Failure to report payments of ownership interest in a timely fashion carries a fine of no more than $10,000 for each payment/interest not disclosed, up to $150,000 per year. Knowing failure to report carries a fine of up to $100,000 per payment/interest not disclosed, up to $1 million per year.
REFERENCES:
Full text of the PPACA and amendments: www.healthcare.gov/law/full/index.html
Supreme Court of the United States, PPACA Cases: www.supremecourt.gov/docket/PPAACA.aspx [sic]
PPACA transcripts: www.supremecourt.gov/oral_arguments/argument_transcripts.aspx
Dear Members and Subscribers,
We are compelled to re-share this succinct summary of the 234,812-word Patient Protection and Affordable Care Act (PPACA). While several elements have been and continue to be modified, the overall constitutionality of its contents are under review by the U.S. Supreme Court. Many are chiming in to offer their...
Dear Members and Subscribers,
We are compelled to re-share this succinct summary of the 234,812-word Patient Protection and Affordable Care Act (PPACA). While several elements have been and continue to be modified, the overall constitutionality of its contents are under review by the U.S. Supreme Court. Many are chiming in to offer their predictions on its fate. We possess no crystal ball through which to forecast our future, but we can provide this digestible version of the Act along with continued, concise reporting of its impact.
Summary of the Patient Protection and Affordable Care Act: QUALITY, AFFORDABLE HEALTH CARE FOR ALL AMERICANS
Immediate Improvements in Health Care Coverage for All Americans
Expand Coverage/Improve Access
Mandate that employers with more than 200 employees automatically enroll employees in health insurance plans offered by the employer (employees may opt out). (2014) Companies with 50 or fewer employees are exempt from fees.
Those with fewer than 200 employees do not have to offer coverage; however, those with more than 50 employees must pay a fee ($2,000 for each full-time employee excluding the first 30) if even one of their full-time employees is receiving a government subsidy for private insurance. Employers with more than 50 employees that offer coverage and have employees receiving subsidies can pay the lower of $3,000 per employee receiving a subsidy or $2,000 per full-time employee.
Provide tax credits to smaller employers (25 or fewer employees and average annual wages of less than $50,000) for purchasing employee health insurance (2010-2013). The employer must contribute at least 50% of total premium cost or an amount to be established by the government. The size of the credit will vary based on company size, i.e., companies with 10 or fewer employees and average annual wages of less than $25,000 get a credit equal to 35% of the employer’s contribution to insurance costs. In 2014 and beyond, the tax credit increases to a maximum of 50% of the employer’s contribution.
Limit the deductible in insurance plans for small groups to no more than $2,000 for individuals and $4,000 for families unless offset by contributions offered by the insurance plan. (2014)
Prohibit cancellation of private insurance coverage except in cases of fraud. (September 2010)
Prohibit denial of coverage based on a pre-existing condition.
Prohibit insurers from refusing coverage for patients who have “consumed” a dollar value of services greater than a pre-determined lifetime limit. (2014)
Expand Medicaid to all individuals under 65 with incomes at or below 133% of the Federal Poverty Level ($10,830 for individuals and $22,050 for a family of four). (Prior to this legislation, not all low-income individuals could avail themselves of Medicaid and eligibility varied from state to state.)
Provide premium credits and cost-sharing subsidies to individuals and families who fall below 400% of the Federal Poverty Level, with some restrictions. (2014)
Establish state-based health exchanges to allow individuals and businesses with fewer than 100 employees to pool together to purchase insurance (2014), with larger businesses (100+ employees) able to participate in 2017. The Federal Government will also offer subsidies to low-income individuals to purchase insurance through the exchanges.
Offer (Federal government through private insurers) at least two multi-state health insurance plans in each state health insurance exchange, with at least one being a non-profit entity. (2014)
Allow parents to keep their children on their health insurance plans up to age 26. (September 2010)
Reduce Costs/Reform Government Programs
Reduce Medicare payments to hospitals by adjusting reimbursement increases to below the market basket beginning with a 1/4 percentage point reduction in 2010 and 2011. (0.1% in 2012 and 2013, 0.2% in 2015 and 2016, and 0.75% in 2017-2019)
Reduce payments to inpatient, outpatient and ASC facilities beginning in 2012.
Apply a productivity reduction to future Medicare payment updates.
Reduce by 75% Medicare and Medicaid payments to “disproportionate share hospitals” (hospitals that care for more costly indigent patients). (2014)
Create the Independent Payment Advisory Board to hold growth in Medicare spending per beneficiary to a certain level. Recommendations from the Board are due by 1/15/2014, with implementation in 2015 unless Congress comes up with its own mechanism for bringing costs in line. Limit growth to GDP growth per capita plus one percentage point beginning in 2018.
Adjust Medicare Advantage payments downward. (2011) (Approximately 25% of Medicare beneficiaries now avail themselves of the Advantage program, paying more to receive additional benefits beyond those provided with basic Medicare coverage.)
Prohibit new physician-owned hospitals, with expansion of existing hospitals requiring approval from the Secretary of HHS. (December 31, 2010)
Require the Secretary of HHS to evaluate and adjust “misvalued” Relative Value Units with a view to corralling those that are the fastest growing in utilization; reflect new technologies or services; have low relative values… (Immediately)
Encourage hospitals and doctors to organize as accountable care organizations (ACOs) to provide coordinated care, encourage investment in infrastructure and increase quality and efficiency by redesigning healthcare delivery processes. (2012) If the ACO saves money, Medicare will share the savings with the ACO, with the ACO distributing savings to its participating hospitals and physicians.
Investigate using a single payment for all services involved in an episode of care for certain treatments (to be chosen by the Secretary of HHS) with the goal to reduce the cost of treatment while not reducing quality. (Medicaid 2012, Medicare 2013)
Extend gainsharing demonstration projects through 2011.
Improve Quality
Expand comparative effectiveness research program (now the Patient-Centered Outcomes Research Institute) and its funding. Note that the legislation indicates that the Institute may not create treatment mandates or practice guidelines nor can it make recommendations for payment coverage. Also, the legislation specifically mentions using comparative effectiveness research to compare medical devices. (Immediately)
Establish the Medicare Innovation Center with $1 billion/year in funding, to test different payment systems to reduce cost and improve quality. (2011)
Mandate physician participation in the Physician Quality Reporting Initiative and penalize physicians who do not satisfactorily report by imposing a 1.5% cut in pay in 2015 and 2% in 2016 and thereafter.
Add a value-based modifier to physicians’ Medicare fee schedule calculation based on quality and cost of treatment to redistribute money to the most cost-efficient physicians. (2017)
Mandate that private insurers (on all health plans) spend a specified proportion of premium dollars (80% or 85% depending on the market being serviced) on clinical services and quality enhancements or measures. (2011)
Add a 1% payment penalty to those hospitals that rank in the top 25% for hospital-acquired conditions; to be applied each year. (2015)
Reduce DRG payments to hospitals deemed to have “excess” readmissions (as determined by HHS), with a 1% reduction in 2013, moving to 3% by 2015.
Redistribute money to the most cost-efficient hospitals based on high quality scores or improvement in scores (calculated based on certain quality measures and cost per beneficiary for certain procedures as determined by HHS). Medicare will pay for the incentives by decreasing base DRG amounts for the procedures, beginning with a 1% reduction in 2013 and ramping to a total 2% reduction in 2017. (Similar programs may be developed for ASCs, SNFs and home health agencies. HHS must report to Congress on these initiatives by 1/1/11.)
Increase Focus on Wellness/Prevention
Mandate that private health plans provide coverage, with no out-of-pocket expense, of “proven” preventive services and immunizations, preventive care for children and adolescents and certain additional preventive care and screenings for women. (2010) A similar mandate takes effect for Medicare and Medicaid in 2011.
Promote wellness programs through incentives to employers, e.g. grants to small employers who establish wellness programs (2011) and ability of larger employers to offer their employees rewards like premium discounts if they participate in wellness programs and meet certain requirements. (2014)
Promote growth in the supply of primary care physicians by paying a 10% bonus to primary care physicians for five years. (2011-2015) (May also be seen as a way to reduce costs, since patients may not require specialist care.)
Promote growth in the supply of general surgeons with a 10% bonus to general surgeons for major surgical procedures in geographies deemed to have a shortage of general surgeons. (2011-2015) (May also be seen as a way to reduce costs, since patients may not require specialist care.)
Redistribute unused residency positions to primary care and general surgery and use
scholarships and loans to support training of primary care physicians. (2010)
Funding the Program
Mandate that all individuals purchase health insurance and impose a fine of $695 per individual ($2,085 maximum per family) for those who do not. Fines may not exceed 2.5% of taxable income. (2014)
Impose a tax deductible medical device fee of 2.3% of U.S. sales of non-retail medical devices to be paid by manufacturers. (Calendar year 2013 revenues)
Impose a 40% fee on insurance companies for “Cadillac” plans, those that offer an aggregate value of more than $10,200 for individuals or $27,500 for family coverage, with the 40% applied to every dollar in value over these amounts. (2018)
Impose fees of $47.5 billion on private insurance companies from 2014 to 2018, as well as an aggregate of $25 billion from 2014 to 2016 to fund a temporary reinsurance program to cover high-risk individuals with pre-existing conditions. After 2018, companies must pay what they paid in the previous year increased by the rate of premium growth.
Impose $16.7 billion in fees on pharmaceutical companies from 2013 to 2019, and $2.8 billion per year thereafter.
Require that pharmaceutical companies provide deeper discounts and rebates for drugs sold to Medicare and Medicaid.
Increase to 2.35% (from 1.45%) the Medicare withholding tax on individuals who make more than $200,000, and joint filers making more than $250,000. (2013)
Impose a 3.8% tax for capital gains and other unearned income on individuals earning more than $200,000 and joint filers making more than $250,000. (2013)
Limit to $500,000 the amount of an individual’s pay that health care insurance companies may deduct as a business expense. (2010)
Transparency – Physician Payment Sunshine Provisions
The “Sunshine” provisions mandate that manufacturers disclose electronically the following information to the government:
All transfers of value to health care providers including individual payments of $10 or more or aggregate payments of $100 or more. (2012) After 2012, amounts will increase by the CPI. Manufacturers need not disclose product samples for patient use, educational materials for patient use, loans of evaluation devices, discounts and rebates, in-kind charity items, profit distributions from publicly-traded securities, health benefits to providers who are employees and payment for non-medical services to licensed non-medical professionals. Furthermore, disclosure of clinical research and product development agreements may be delayed until the product has been cleared for marketing or four years after the date of payment to the healthcare provider, whichever is earlier.
Ownership or investment interest (other than an ownership or investment interest in a publicly traded security and mutual fund) held by a physician (or an immediate family member of such physician) in the applicable manufacturer or applicable group purchasing organization during the preceding year.
Failure to report payments of ownership interest in a timely fashion carries a fine of no more than $10,000 for each payment/interest not disclosed, up to $150,000 per year. Knowing failure to report carries a fine of up to $100,000 per payment/interest not disclosed, up to $1 million per year.
REFERENCES:
Full text of the PPACA and amendments: www.healthcare.gov/law/full/index.html
Supreme Court of the United States, PPACA Cases: www.supremecourt.gov/docket/PPAACA.aspx [sic]
PPACA transcripts: www.supremecourt.gov/oral_arguments/argument_transcripts.aspx

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
ME
Mike Evers is a Senior Market Analyst and writer with over 15 years of experience in the medical industry, spanning cardiac rhythm management, ER coding and billing, and orthopedics. He joined ORTHOWORLD in 2018, where he provides market analysis and editorial coverage.