
 Copy to clipboard
Copy to clipboard 
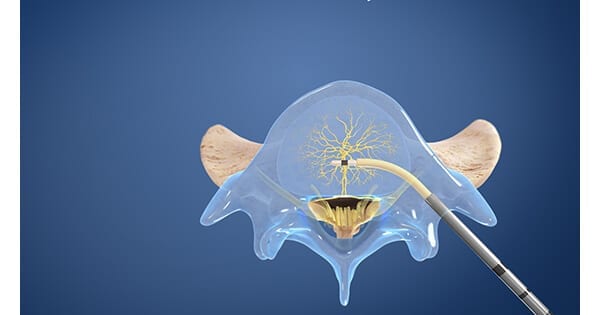
Relievant Medsystems announced 12-month results from a Level 1 prospective randomized multi-center trial that demonstrated the effectiveness and superiority of the Intracept® Procedure for vertebrogenic chronic lower back pain compared to standard care treatments.
The INTRACEPT study randomized 140 patients across 20 sites and enrollment was stopped early due to statistical superiority at the pre-specified interim analysis; primary results were published in 2019, showing a significant difference between the Intracept arm and the standard care arm for the primary endpoint and all secondary endpoints at three months post-procedure.
The newly published data report outcomes for the full randomized trial cohort, including six-month between arm comparisons, 12-month treatment arm results, and six-month outcomes post-procedure for patients in the prior standard care arm that elected to crossover and receive basivertebral nerve (BVN) ablation upon the trial enrollment being stopped.
The published results demonstrate a 24.5 difference between arms in reduction in mean ODI, with BVN ablation arm (26.1 points, p<0.001) versus standard care arm (1.6 points, p<0.001) at six months post-procedure, validating superiority of the Intracept Procedure compared to standard care.
These outcomes continued through 12 months, with statistically significant and clinically meaningful reductions in mean ODI (25.7 points, p<0.001) and mean VAS (3.8 cm, p<0.001) from baseline through 12 months in the Intracept treatment arm.
Additionally, crossover patients who were re-baselined prior to receiving the Intracept procedure reported nearly identical outcomes, with reductions in mean ODI (25.9 points, p<0.001) and mean VAS (3.8 cm, p<0.001) compared to baseline at six months post-procedure.
Other key results from the study include:
- 64% of patients in the Intracept treatment arm reported ≥50% reduction in pain, while 30% reported they had complete pain resolution at 12 months; similar reductions in pain were reported in crossover patients at six months post-procedure.
- 92% of patients in the Intracept treatment arm who had epidural steroid injections prior to treatment did not have any injections in the 12 months after treatment. Crossover patients reported a 100% reduction in injections six months post-procedure.
- 74% of patients in the Intracept treatment arm reported improvement of their condition, with 75% indicating treatment success at 12 months. Former standard care patients who crossed over to BVN ablation reported similar satisfaction at six months post-procedure (78% improvement, 72% success).
There were no serious device or procedure-related adverse events.
“The positive outcomes from the full cohort of the INTRACEPT randomized trial add to the significant portfolio of long-term evidence post-BVN ablation, with patients in the BVN ablation arm showing consistent outcomes with prior long-term studies,” said Tyler Binney, President & CEO, Relievant Medsystems. “Following the publication of positive 5-year data from the SMART trial, these results further demonstrate that outcomes post-Intracept procedure are long-lasting, reproducible, and superior to standard care – with the potential to positively improve the lives of the millions of patients suffering from chronic vertebrogenic low back pain.”
Source: Relievant Medsystems
Relievant Medsystems announced 12-month results from a Level 1 prospective randomized multi-center trial that demonstrated the effectiveness and superiority of the Intracept® Procedure for vertebrogenic chronic lower back pain compared to standard care treatments.
The INTRACEPT study randomized 140 patients across 20 sites and enrollment was...
Relievant Medsystems announced 12-month results from a Level 1 prospective randomized multi-center trial that demonstrated the effectiveness and superiority of the Intracept® Procedure for vertebrogenic chronic lower back pain compared to standard care treatments.
The INTRACEPT study randomized 140 patients across 20 sites and enrollment was stopped early due to statistical superiority at the pre-specified interim analysis; primary results were published in 2019, showing a significant difference between the Intracept arm and the standard care arm for the primary endpoint and all secondary endpoints at three months post-procedure.
The newly published data report outcomes for the full randomized trial cohort, including six-month between arm comparisons, 12-month treatment arm results, and six-month outcomes post-procedure for patients in the prior standard care arm that elected to crossover and receive basivertebral nerve (BVN) ablation upon the trial enrollment being stopped.
The published results demonstrate a 24.5 difference between arms in reduction in mean ODI, with BVN ablation arm (26.1 points, p<0.001) versus standard care arm (1.6 points, p<0.001) at six months post-procedure, validating superiority of the Intracept Procedure compared to standard care.
These outcomes continued through 12 months, with statistically significant and clinically meaningful reductions in mean ODI (25.7 points, p<0.001) and mean VAS (3.8 cm, p<0.001) from baseline through 12 months in the Intracept treatment arm.
Additionally, crossover patients who were re-baselined prior to receiving the Intracept procedure reported nearly identical outcomes, with reductions in mean ODI (25.9 points, p<0.001) and mean VAS (3.8 cm, p<0.001) compared to baseline at six months post-procedure.
Other key results from the study include:
- 64% of patients in the Intracept treatment arm reported ≥50% reduction in pain, while 30% reported they had complete pain resolution at 12 months; similar reductions in pain were reported in crossover patients at six months post-procedure.
- 92% of patients in the Intracept treatment arm who had epidural steroid injections prior to treatment did not have any injections in the 12 months after treatment. Crossover patients reported a 100% reduction in injections six months post-procedure.
- 74% of patients in the Intracept treatment arm reported improvement of their condition, with 75% indicating treatment success at 12 months. Former standard care patients who crossed over to BVN ablation reported similar satisfaction at six months post-procedure (78% improvement, 72% success).
There were no serious device or procedure-related adverse events.
“The positive outcomes from the full cohort of the INTRACEPT randomized trial add to the significant portfolio of long-term evidence post-BVN ablation, with patients in the BVN ablation arm showing consistent outcomes with prior long-term studies,” said Tyler Binney, President & CEO, Relievant Medsystems. “Following the publication of positive 5-year data from the SMART trial, these results further demonstrate that outcomes post-Intracept procedure are long-lasting, reproducible, and superior to standard care – with the potential to positively improve the lives of the millions of patients suffering from chronic vertebrogenic low back pain.”
Source: Relievant Medsystems

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
JV
Julie Vetalice is ORTHOWORLD's Editorial Assistant. She has covered the orthopedic industry for over 20 years, having joined the company in 1999.