Copy to clipboard
Copy to clipboard 
Cerapedics announced today that results of a study to evaluate the cost-effectiveness of i-FACTOR Peptide Enhanced Bone Graft compared to autograft for patients undergoing ACDF surgery were recently published in ClinicoEconomics and Outcomes Research (July 2021, Volume 2021, Issue 13). In this landmark study, the data demonstrates that i-FACTOR was cost-effective compared to local autograft in ACDF surgery.
The patient cohort was extracted from a prospective, multicenter randomized control trial (R.C.T.) from 22 North American centers. The study analyzed various real-world scenarios, including inpatient and outpatient surgical settings and private versus public insurances. Two primary outcome measures were assessed: cost and utility. In the base-case analysis, both health and societal system costs were evaluated.
“In a robust cost-utility analysis, i-FACTOR reduced costs within the first year compared to the control group (autograft) in the ACDF IDE trial population. The incremental cost-effectiveness ratio proved highly cost-effective even at 90 days ($13,333 per QALY). At 1 year and beyond, these values became negative, suggesting a ‘dominant’ economic strategy. The results are felt to be conservative since, in a real world setting, many surgeons are using other more costly grafts in addition to autograft,” commented study leader Dr. Jared Ament, M.D., M.P.H., Director of Outcomes Research and Co-Director of Spine Neurosurgery at the Neurosurgery & Spine Group (N.S.G.) and President and Founder of Neuronomics.
i-FACTOR has already demonstrated safety and improved outcomes compared to local autograft based on one- and two-year published data in Spine & Neurosurgery Journals. This comprehensive, cost-effectiveness analysis was the next critical and necessary step to provide clear support for a better alternative to autograft.
“We are grateful to Dr. Ament and his team for conducting this important and infrequently conducted analysis. As our healthcare system becomes ever more focused on value in addition to quality clinical outcomes, this data puts us in a unique position relative to our competition. The technologies we displace with i-FACTOR don’t have cost-effectiveness data, and most have no meaningful clinical data as well,” said Jeffrey G. Marx, Ph.D., President, and Chief Operating Officer.
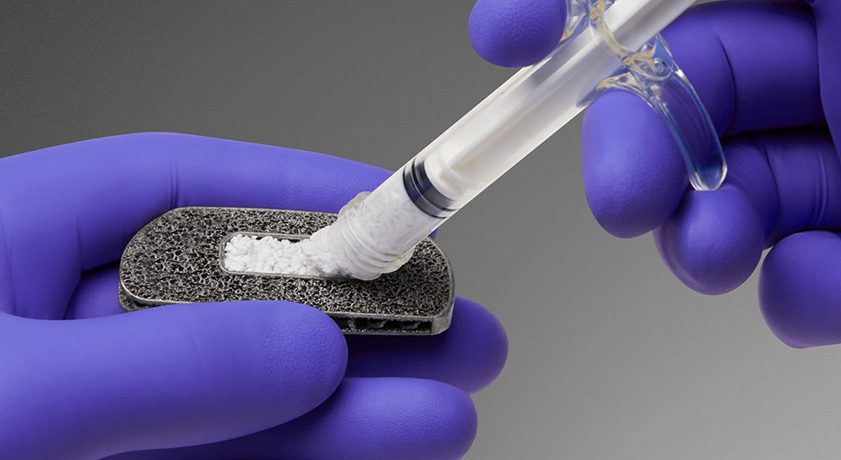
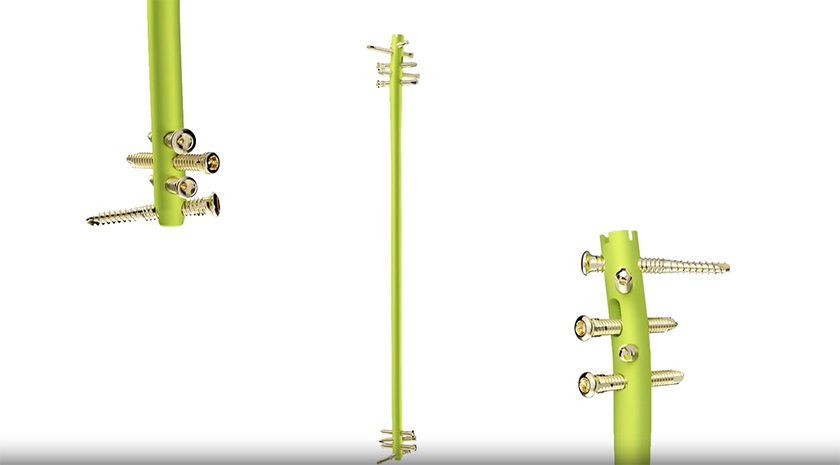
i-FACTOR bone graft has over 10 years of clinical success in Europe and was approved in the U.S. for use in ACDF procedures in 2015. The drug-device combination product is based on small peptide (P-15) technology that accelerates new bone formation in patients with degenerative disc disease. It is in a new category of bone graft technology and is one of only two drug-device combination products approved by FDA. In 2018, the company enrolled the first patients in an IDE clinical trial evaluating the safety and efficacy of its next-generation product, P-15L Peptide Enhanced Bone Graft, for use in patients undergoing TLIF.
Source: Cerapedics
Cerapedics announced today that results of a study to evaluate the cost-effectiveness of i-FACTOR Peptide Enhanced Bone Graft compared to autograft for patients undergoing ACDF surgery were recently published in ClinicoEconomics and Outcomes Research (July 2021, Volume 2021, Issue 13). In this landmark study, the data demonstrates that i-FACTOR...
Cerapedics announced today that results of a study to evaluate the cost-effectiveness of i-FACTOR Peptide Enhanced Bone Graft compared to autograft for patients undergoing ACDF surgery were recently published in ClinicoEconomics and Outcomes Research (July 2021, Volume 2021, Issue 13). In this landmark study, the data demonstrates that i-FACTOR was cost-effective compared to local autograft in ACDF surgery.
The patient cohort was extracted from a prospective, multicenter randomized control trial (R.C.T.) from 22 North American centers. The study analyzed various real-world scenarios, including inpatient and outpatient surgical settings and private versus public insurances. Two primary outcome measures were assessed: cost and utility. In the base-case analysis, both health and societal system costs were evaluated.
“In a robust cost-utility analysis, i-FACTOR reduced costs within the first year compared to the control group (autograft) in the ACDF IDE trial population. The incremental cost-effectiveness ratio proved highly cost-effective even at 90 days ($13,333 per QALY). At 1 year and beyond, these values became negative, suggesting a ‘dominant’ economic strategy. The results are felt to be conservative since, in a real world setting, many surgeons are using other more costly grafts in addition to autograft,” commented study leader Dr. Jared Ament, M.D., M.P.H., Director of Outcomes Research and Co-Director of Spine Neurosurgery at the Neurosurgery & Spine Group (N.S.G.) and President and Founder of Neuronomics.
i-FACTOR has already demonstrated safety and improved outcomes compared to local autograft based on one- and two-year published data in Spine & Neurosurgery Journals. This comprehensive, cost-effectiveness analysis was the next critical and necessary step to provide clear support for a better alternative to autograft.
“We are grateful to Dr. Ament and his team for conducting this important and infrequently conducted analysis. As our healthcare system becomes ever more focused on value in addition to quality clinical outcomes, this data puts us in a unique position relative to our competition. The technologies we displace with i-FACTOR don’t have cost-effectiveness data, and most have no meaningful clinical data as well,” said Jeffrey G. Marx, Ph.D., President, and Chief Operating Officer.
i-FACTOR bone graft has over 10 years of clinical success in Europe and was approved in the U.S. for use in ACDF procedures in 2015. The drug-device combination product is based on small peptide (P-15) technology that accelerates new bone formation in patients with degenerative disc disease. It is in a new category of bone graft technology and is one of only two drug-device combination products approved by FDA. In 2018, the company enrolled the first patients in an IDE clinical trial evaluating the safety and efficacy of its next-generation product, P-15L Peptide Enhanced Bone Graft, for use in patients undergoing TLIF.
Source: Cerapedics

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
JV
Julie Vetalice is ORTHOWORLD's Editorial Assistant. She has covered the orthopedic industry for over 20 years, having joined the company in 1999.