
 Copy to clipboard
Copy to clipboard 
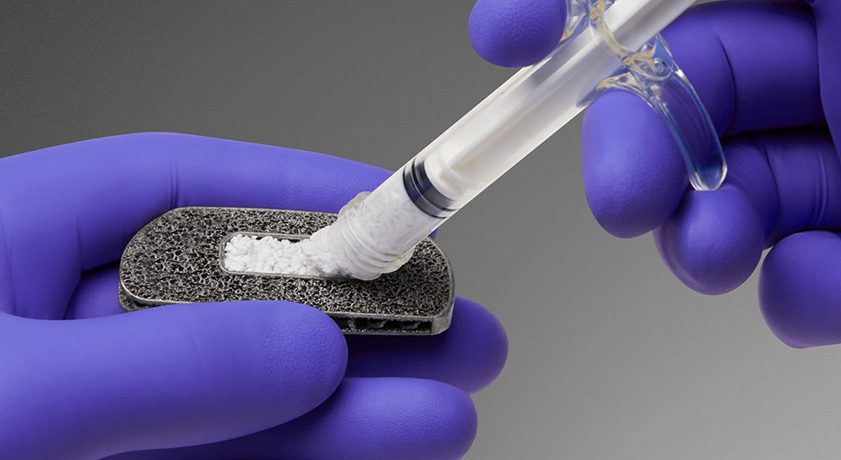
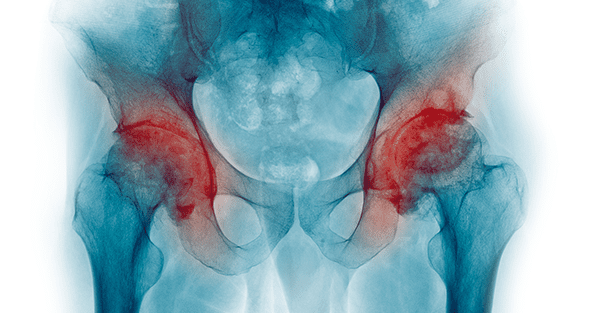
Hip Innovation Technology (HIT) presented data demonstrating the potential utility of its novel Reverse Hip Replacement System (Reverse HRS) in addressing instability following total hip arthroplasty (THA).
Researchers reported Phase I data showing radiographic stability, as assessed by radio-stereometric analysis in patients who underwent THA with the Reverse HRS. Results suggest a low risk of aseptic loosening of the Reverse HRS, and a high likelihood of long-term implant fixation.
“Instability following total hip arthroplasty is a common mode of failure,” commented lead investigator Thomas Turgeon, MD, Director of Arthroplasty Research, Concordia Hip and Knee Institute and Board Member of the Orthopaedic Innovation Centre. “The Reverse Hip Replacement System is designed to increase stability at the extremes of motion, and to offer a potentially more forgiving implant positioning without reducing range of motion. The clinical outcome metrics we have observed thus far are consistent with well-functioning hip replacement, and support the stability of this novel implant device.”
The data represented findings from 22 patients implanted with the Reverse HRS. The mean 24-month acetabular migration in these patients was 0.09 ± 0.15mm (p=0.005), which compared favorably to the maximum acceptable migration of 0.2mm. Similarly, the mean 24-month femoral migration was 0.002 ± 0.19mm (p<0.001), compared to the maximal acceptable migration of 0.5mm. At 24 months post-THA, the Reverse HRS was also associated with significant improvements in patient-reported outcome measures including the hip disability and osteoarthritis outcome score (HOOS), Oxford Hip Score (OHS), Harris Hip Score (HHS) and the 36-item short-form survey (SF-36) physical score (p<0.001 for all).
“The results from this ongoing RSA assessment trial bolster the clinical rationale for the Reverse HRS and its unique implant design,” said George Diamantoni, Hip Innovation Technology’s Co-Founder and Chief Executive Officer. “The findings further validate and strengthen the importance for our soon to launch FDA-approved IDE pivotal trial, which will evaluate the effectiveness and safety of the Reverse HRS in subjects undergoing primary THA. We believe the potential benefits of the Reverse HRS include hip stability at extended ranges of motion, reduced risk of device dislocation, and greater latitude for placement of hip components.”
Source: Hip Innovation Technology, LLC
Hip Innovation Technology (HIT) presented data demonstrating the potential utility of its novel Reverse Hip Replacement System (Reverse HRS) in addressing instability following total hip arthroplasty (THA).
Researchers reported Phase I data showing radiographic stability, as assessed by radio-stereometric analysis in patients who underwent THA...
Hip Innovation Technology (HIT) presented data demonstrating the potential utility of its novel Reverse Hip Replacement System (Reverse HRS) in addressing instability following total hip arthroplasty (THA).
Researchers reported Phase I data showing radiographic stability, as assessed by radio-stereometric analysis in patients who underwent THA with the Reverse HRS. Results suggest a low risk of aseptic loosening of the Reverse HRS, and a high likelihood of long-term implant fixation.
“Instability following total hip arthroplasty is a common mode of failure,” commented lead investigator Thomas Turgeon, MD, Director of Arthroplasty Research, Concordia Hip and Knee Institute and Board Member of the Orthopaedic Innovation Centre. “The Reverse Hip Replacement System is designed to increase stability at the extremes of motion, and to offer a potentially more forgiving implant positioning without reducing range of motion. The clinical outcome metrics we have observed thus far are consistent with well-functioning hip replacement, and support the stability of this novel implant device.”
The data represented findings from 22 patients implanted with the Reverse HRS. The mean 24-month acetabular migration in these patients was 0.09 ± 0.15mm (p=0.005), which compared favorably to the maximum acceptable migration of 0.2mm. Similarly, the mean 24-month femoral migration was 0.002 ± 0.19mm (p<0.001), compared to the maximal acceptable migration of 0.5mm. At 24 months post-THA, the Reverse HRS was also associated with significant improvements in patient-reported outcome measures including the hip disability and osteoarthritis outcome score (HOOS), Oxford Hip Score (OHS), Harris Hip Score (HHS) and the 36-item short-form survey (SF-36) physical score (p<0.001 for all).
“The results from this ongoing RSA assessment trial bolster the clinical rationale for the Reverse HRS and its unique implant design,” said George Diamantoni, Hip Innovation Technology’s Co-Founder and Chief Executive Officer. “The findings further validate and strengthen the importance for our soon to launch FDA-approved IDE pivotal trial, which will evaluate the effectiveness and safety of the Reverse HRS in subjects undergoing primary THA. We believe the potential benefits of the Reverse HRS include hip stability at extended ranges of motion, reduced risk of device dislocation, and greater latitude for placement of hip components.”
Source: Hip Innovation Technology, LLC

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
JV
Julie Vetalice is ORTHOWORLD's Editorial Assistant. She has covered the orthopedic industry for over 20 years, having joined the company in 1999.