Copy to clipboard
Copy to clipboard 
Clinical studies demonstrated that Stryker’s Mako Total Knee was associated with less pain and need for opiates, shorter hospital stays, improved flexion and soft tissue protection vs. manual techniques.
A prospective, single-surgeon, consecutive series study compared 40 patients undergoing manual total knee arthroplasty (TKA) to an equal number with Mako. The latter group exhibited less post-op pain, a decreased need for opiates, a 26% reduction in length of hospital stay and less need for in-patient physical therapy.
A longitudinal, retrospective analysis of CMS Medicare claims data evaluated the 90-day episode-of-care costs for manual vs. Mako TKA, concluding that Mako patients had overall lower average 90-day costs to Medicare, driven by reduced facility costs, shorter lengths of stay, decreased readmissions, etc.
An additional prospective cohort study compared macroscopic bone/soft tissue injury results between Mako and manual TKA. The study compared 30 consecutive manual TKAs to an equal number of consecutive Mako TKA procedures, performed by a single surgeon. Results indicated reduced bone and soft tissue damage in the Mako patient group.
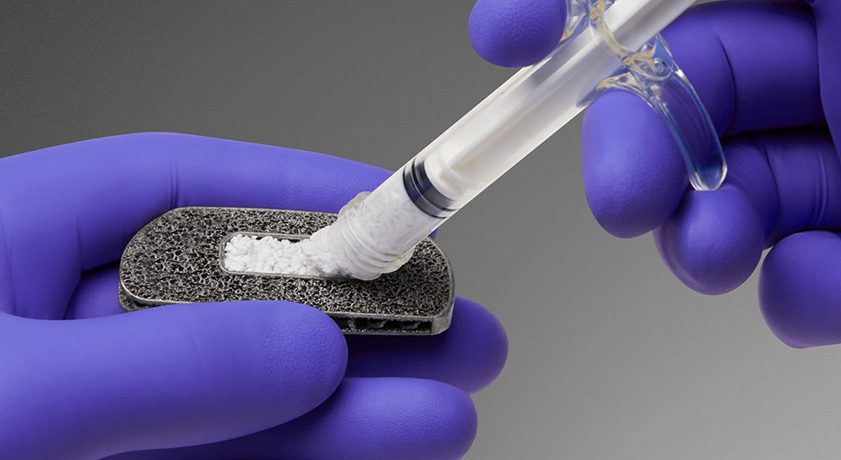
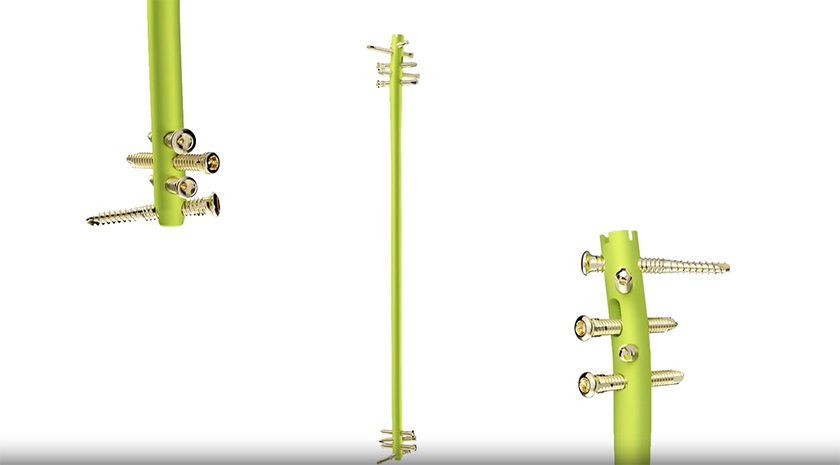
As noted in Stryker’s 4Q18/2018 earnings call, the global total of installed Mako units is 642 (523 in the U.S.), with the majority of these now upgraded to the total knee application. The ability to perform a cementless total knee on the robot is helping drive cementless knee adoption. As of the end of 2018, 30% of all Stryker knees are cementless.
Sources: Stryker Corporation; ORTHOWORLD Inc.
Clinical studies demonstrated that Stryker's Mako Total Knee was associated with less pain and need for opiates, shorter hospital stays, improved flexion and soft tissue protection vs. manual techniques.
A prospective, single-surgeon, consecutive series study compared 40 patients undergoing manual total knee arthroplasty (TKA) to an equal...
Clinical studies demonstrated that Stryker’s Mako Total Knee was associated with less pain and need for opiates, shorter hospital stays, improved flexion and soft tissue protection vs. manual techniques.
A prospective, single-surgeon, consecutive series study compared 40 patients undergoing manual total knee arthroplasty (TKA) to an equal number with Mako. The latter group exhibited less post-op pain, a decreased need for opiates, a 26% reduction in length of hospital stay and less need for in-patient physical therapy.
A longitudinal, retrospective analysis of CMS Medicare claims data evaluated the 90-day episode-of-care costs for manual vs. Mako TKA, concluding that Mako patients had overall lower average 90-day costs to Medicare, driven by reduced facility costs, shorter lengths of stay, decreased readmissions, etc.
An additional prospective cohort study compared macroscopic bone/soft tissue injury results between Mako and manual TKA. The study compared 30 consecutive manual TKAs to an equal number of consecutive Mako TKA procedures, performed by a single surgeon. Results indicated reduced bone and soft tissue damage in the Mako patient group.
As noted in Stryker’s 4Q18/2018 earnings call, the global total of installed Mako units is 642 (523 in the U.S.), with the majority of these now upgraded to the total knee application. The ability to perform a cementless total knee on the robot is helping drive cementless knee adoption. As of the end of 2018, 30% of all Stryker knees are cementless.
Sources: Stryker Corporation; ORTHOWORLD Inc.

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
JV
Julie Vetalice is ORTHOWORLD's Editorial Assistant. She has covered the orthopedic industry for over 20 years, having joined the company in 1999.