
 Copy to clipboard
Copy to clipboard 
Rotator cuff repair has gained attention as an orthopedic procedure with untapped potential. Orthopedic surgeon Stefan Welte, M.D., believes that a better understanding of the body’s biological response will lead to innovative rotator cuff repair solutions that advance patient outcomes and surgical techniques.
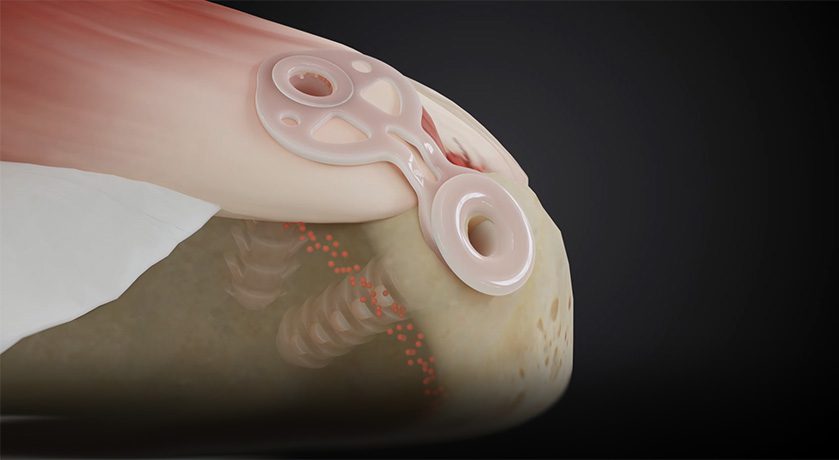
Dr. Welte is the Co-founder of Inovedis and the inventor of the SINEFIX implant. The German startup has approached the problem of high retear rates by designing an implant that makes rotator cuff repair easier and faster. SINEFIX involves a two-step technique that better maintains blood circulation at the site of repair to improve outcomes.
“Rotator cuff repair hasn’t changed much in 20 years, and maybe we need to look to biologics for the next wave of innovation,” Dr. Welte said. “Many surgeons have the same feeling.”
We spoke to Dr. Welte to better understand the intricacies of advancements in rotator cuff repair, the challenges facing traditional sutures and the future trajectory of the surgery.
How do the latest advancements, including those within your company’s product portfolio, address the challenges seen with traditional sutures? What improvements can patients and surgeons expect from those advancements?
Dr. Welte: Our startup has embarked on a focused journey within a narrow portfolio that is centered on the transformative SINEFIX device. Recognizing the limitations of sutures for rotator cuff repair, we sought out a new approach. The SINEFIX implant, crafted from PEEK material, is the culmination of our efforts to introduce a simpler, more effective technique.
Our technology is rooted in the realization that despite various suturing techniques — single row, double row and suture-rich — there seemed to be limited enhancements in rotator cuff repair outcomes. The industry’s emphasis on the biomechanics of technology, while crucial, led us to acknowledge a potential oversight on the biological front. That thought led us to focus on the critical role of blood circulation at the repair site.
There’s an old saying in surgery, “If there’s no blood, there’s no life.” Implants that share the force of the tension between bone and tendon and maintain blood circulation provide better results than the use of sutures alone. This strategic departure minimizes punctual pressure, reducing the risk of loosening during the crucial initial weeks post-surgery.
As we shift the market’s perspective, patients and surgeons can anticipate reduced retear and failure rates. The SINEFIX implant simplifies the surgical process and addresses the biological nuances that are often overlooked. This holistic approach endeavors to elevate the standards of rotator cuff repair, promising enhanced outcomes and a more resilient solution for patients and surgeons alike.
The SINEFIX implant is made of PEEK. How does your choice of material contribute to the implant’s improved strength and biocompatibility?
Dr. Welte: PEEK is known for its biocompatibility and compatibility with imaging techniques. The material boasts favorable mechanical properties that resemble the stiffness of bone and demonstrate robust resistance to environmental stress cracking. Plus, unlike metals often used in implants, the polymer allows for postoperative MRI scans, which provide surgeons valuable insights into the patient’s healing process.
The foundation of our product development, particularly the SINEFIX implant, is rooted in a paradigm shift toward a biologically informed approach to rotator cuff repair. To further address high failure rates, we are exploring new materials with the goal of potentially creating an implant out of biologic materials that can better promote healing.
How do your products, particularly the SINEFIX implant, contribute to the development of minimally invasive rotator cuff repair techniques? What advantages do these techniques offer to surgeons and patients?
Dr. Welte: The SINEFIX implant was designed with simplicity in mind. It isn’t always easy for surgeons who don’t specialize in rotator cuff repair to handle and place suture anchors. Tying knots around two, three or four sutures requires some skill. It can be quite time-consuming. The easier the technique, the less room there is for error.
Our two-step technique not only addresses biomechanics, but also ensures ease of use. This makes the implant suitable for a broader range of surgeons, reduces procedure times and benefits surgeons and patients. The emphasis is on accessibility without compromising efficacy.
How do you envision rotator cuff repair evolving over the next five years, considering the current challenges and advancements in technology?
Dr. Welte: The surgery holds immense potential for transformative change. There is a growing consensus among surgeons, myself included, that a more profound exploration of biology is warranted. The traditional fixation with biomechanics — akin to using a hammer and screw — needs reevaluation. Surgeons recognize the need to transcend a mechanistic garage-like approach and delve deeper into the body’s natural healing processes.
We need to focus more on repair techniques and biologic treatments and less on biomechanical devices. The body’s healing process is complex, and we’re still far away from understanding its mechanisms. We need to discover how to give the body what it needs in the best way.
Rotator cuff repair has gained attention as an orthopedic procedure with untapped potential. Orthopedic surgeon Stefan Welte, M.D., believes that a better understanding of the body’s biological response will lead to innovative rotator cuff repair solutions that advance patient outcomes and surgical techniques.
Dr. Welte is the Co-founder of...
Rotator cuff repair has gained attention as an orthopedic procedure with untapped potential. Orthopedic surgeon Stefan Welte, M.D., believes that a better understanding of the body’s biological response will lead to innovative rotator cuff repair solutions that advance patient outcomes and surgical techniques.
Dr. Welte is the Co-founder of Inovedis and the inventor of the SINEFIX implant. The German startup has approached the problem of high retear rates by designing an implant that makes rotator cuff repair easier and faster. SINEFIX involves a two-step technique that better maintains blood circulation at the site of repair to improve outcomes.
“Rotator cuff repair hasn’t changed much in 20 years, and maybe we need to look to biologics for the next wave of innovation,” Dr. Welte said. “Many surgeons have the same feeling.”
We spoke to Dr. Welte to better understand the intricacies of advancements in rotator cuff repair, the challenges facing traditional sutures and the future trajectory of the surgery.
How do the latest advancements, including those within your company’s product portfolio, address the challenges seen with traditional sutures? What improvements can patients and surgeons expect from those advancements?
Dr. Welte: Our startup has embarked on a focused journey within a narrow portfolio that is centered on the transformative SINEFIX device. Recognizing the limitations of sutures for rotator cuff repair, we sought out a new approach. The SINEFIX implant, crafted from PEEK material, is the culmination of our efforts to introduce a simpler, more effective technique.
Our technology is rooted in the realization that despite various suturing techniques — single row, double row and suture-rich — there seemed to be limited enhancements in rotator cuff repair outcomes. The industry’s emphasis on the biomechanics of technology, while crucial, led us to acknowledge a potential oversight on the biological front. That thought led us to focus on the critical role of blood circulation at the repair site.
There’s an old saying in surgery, “If there’s no blood, there’s no life.” Implants that share the force of the tension between bone and tendon and maintain blood circulation provide better results than the use of sutures alone. This strategic departure minimizes punctual pressure, reducing the risk of loosening during the crucial initial weeks post-surgery.
As we shift the market’s perspective, patients and surgeons can anticipate reduced retear and failure rates. The SINEFIX implant simplifies the surgical process and addresses the biological nuances that are often overlooked. This holistic approach endeavors to elevate the standards of rotator cuff repair, promising enhanced outcomes and a more resilient solution for patients and surgeons alike.
The SINEFIX implant is made of PEEK. How does your choice of material contribute to the implant’s improved strength and biocompatibility?
Dr. Welte: PEEK is known for its biocompatibility and compatibility with imaging techniques. The material boasts favorable mechanical properties that resemble the stiffness of bone and demonstrate robust resistance to environmental stress cracking. Plus, unlike metals often used in implants, the polymer allows for postoperative MRI scans, which provide surgeons valuable insights into the patient’s healing process.
The foundation of our product development, particularly the SINEFIX implant, is rooted in a paradigm shift toward a biologically informed approach to rotator cuff repair. To further address high failure rates, we are exploring new materials with the goal of potentially creating an implant out of biologic materials that can better promote healing.
How do your products, particularly the SINEFIX implant, contribute to the development of minimally invasive rotator cuff repair techniques? What advantages do these techniques offer to surgeons and patients?
Dr. Welte: The SINEFIX implant was designed with simplicity in mind. It isn’t always easy for surgeons who don’t specialize in rotator cuff repair to handle and place suture anchors. Tying knots around two, three or four sutures requires some skill. It can be quite time-consuming. The easier the technique, the less room there is for error.
Our two-step technique not only addresses biomechanics, but also ensures ease of use. This makes the implant suitable for a broader range of surgeons, reduces procedure times and benefits surgeons and patients. The emphasis is on accessibility without compromising efficacy.
How do you envision rotator cuff repair evolving over the next five years, considering the current challenges and advancements in technology?
Dr. Welte: The surgery holds immense potential for transformative change. There is a growing consensus among surgeons, myself included, that a more profound exploration of biology is warranted. The traditional fixation with biomechanics — akin to using a hammer and screw — needs reevaluation. Surgeons recognize the need to transcend a mechanistic garage-like approach and delve deeper into the body’s natural healing processes.
We need to focus more on repair techniques and biologic treatments and less on biomechanical devices. The body’s healing process is complex, and we’re still far away from understanding its mechanisms. We need to discover how to give the body what it needs in the best way.

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
KK
Kendal Kloiber is an ORTHOWORLD Contributor.







